Taking Sick
On Jan 15, 1998 ZetaTalk stated that Illness will increase as Planet X approaches. Zetas right again !!!
- ZetaTalk: Take Sick, written Feb 15, 1998.
- Increasingly, as the pole shift nears, the populace will take sick. This will take the form of known illnesses occurring more frequently, seemingly depressed immune systems, but will also appear as new and puzzling illnesses not seen before in the memory of man. What is going on here?
The changes at the core of the Earth that have resulted in El Nino weather patterns and white buffalo and deformed frogs also affect man. The germs are on the move. Their carriers are on the move. And thus humans are exposed to diseases that are so rare as to be undocumented in medical journals.
You will see increasing illness, odd illnesses, microbes that travel because an insect is scattering about and spreading germs in places where it normally doesn't travel. 90% of all the illness and distress you're going to see is a natural situation, a natural occurrence. Because of the changing, swirling in the core of the Earth, and this will continue to up-tick until the pole shift.
And reiterated in 1999
- ZetaTalk: Next 3 1/2 Years, written Sep 15, 1999.
- Sickness will slightly increase from where it is today. There is a lot of illness now because people who are already unstable are unable to take the turmoil caused by the increased emanations from the Earth. Some of them have simply sensed what is coming and have decided to die. This is true of animals as well as humans. Sickness will increase, but not to the point where it is going to get exponentially worse.
On Feb 2, 2000 a Washington report confirmed this increase, and published concerns were subsequently reported.
- Diseases From Around World Threatening U.S.
Reuters, Feb 2, 2000
- 30 New Diseases Make Global Debut
At least 30 previously unknown diseases have appeared globally since 1973, including HIV, AIDS, Hepatitis C, Ebola haemorrhagic fever and the encephalitis-related Nipah virus that emerged in Indonesia. Twenty well-known infectious diseases such as tuberculosis, malaria, and cholera have re-emerged or spread since 1973.
-
- Is Global Warming Harmful to Health?
Scientific American, August 2000
- Notably, computer models predict that global warming, and other climate alterations it induces, will expand the incidence and distribution of many serious medical disorders. Disturbingly, these forecasts seem to be coming true.
And since this time, SARS and increased incidence of flesh eating disease,
and entire cruise ships regularly returning to port with the passengers ill with stomach flu have been reported.
Depressed immune systems?
Zetas RIGHT Again!
After the pole shift, there will be many opportunistic diseases that will afflict mankind. This does not require an imagination, as today they afflict mankind after disasters. The primary affliction will be from sewage laden water, which will pollute the drinking water man is forced to use. We have been adamant about mankind distilling their drinking water after the pole shift for this reason. Distillation removes heavy metals as well as killing microbes by the boiling process. Any disease that flourishes in malnourished bodies and in areas of poor hygiene will take advantage of the pole shift disasters. Scurvy due to lack of Vitamin C will occur, with bleeding gums and even death if not corrected. Many weeds are high in Vitamin C and survivors should arm themselves with knowledge about the vitamin content of weeds. Unprotected sex by survivors either taking advantage of the weak, as in rape, or by simple distraction and grief and a lack of contraceptive devices will spread AIDS and hepatitis. Morgellons, which is caused by a synergy of parasites and microbes when the immune system is low will likely increase. There will be outbreaks of diseases which were endemic in the past, such as small pox or measles, but in those survivor communities where the members have been immunized in the past these will be limited and quarantines can help in this regard.
http://www.zetatalk5.com/ning/20no2010.htm
Chile battles youth unrest and typhoid fever outbreak
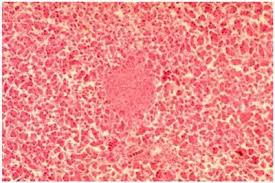 September 15, 2011 – SANTIAGO – Chile’s problems dealing with youth unrest over slow education reforms are being compounded by concerns the capital may be in the grip of a typhoid fever outbreak. The government has battled to enforce restraint on law enforcement agencies amid angry student-led protests, which have disrupted urban centers across the country for more than a month. The reforms demanded by youth groups are nowhere near being implemented and protests continue to simmer with support from teachers and workers unions. Now authorities are faced with the more immediate risk of typhoid. Health authorities issued repeated alerts for tougher hygiene checks and controls after they found several people infected and seriously ill with typhoid in the western metropolitan area of Santiago. At least seven cases were confirmed by the Public Health Institute but there were no immediate reports of fatalities. “Typhoid fever is an acute infectious disease triggered by a salmonella bacteria strain,” Institute Director Maria Teresa Valenzuela said. In most cases the infection is caused by consumption of contaminated food and drink or fruit and vegetables grown in areas where contaminated water is used in irrigation. Typhoid fever produces symptoms of high fever, diarrhea or intense headaches. The Santiago region has been prone to typhoid outbreaks since the 1990s when incidence of the disease caused up to 190 cases a year.
September 15, 2011 – SANTIAGO – Chile’s problems dealing with youth unrest over slow education reforms are being compounded by concerns the capital may be in the grip of a typhoid fever outbreak. The government has battled to enforce restraint on law enforcement agencies amid angry student-led protests, which have disrupted urban centers across the country for more than a month. The reforms demanded by youth groups are nowhere near being implemented and protests continue to simmer with support from teachers and workers unions. Now authorities are faced with the more immediate risk of typhoid. Health authorities issued repeated alerts for tougher hygiene checks and controls after they found several people infected and seriously ill with typhoid in the western metropolitan area of Santiago. At least seven cases were confirmed by the Public Health Institute but there were no immediate reports of fatalities. “Typhoid fever is an acute infectious disease triggered by a salmonella bacteria strain,” Institute Director Maria Teresa Valenzuela said. In most cases the infection is caused by consumption of contaminated food and drink or fruit and vegetables grown in areas where contaminated water is used in irrigation. Typhoid fever produces symptoms of high fever, diarrhea or intense headaches. The Santiago region has been prone to typhoid outbreaks since the 1990s when incidence of the disease caused up to 190 cases a year.
http://theextinctionprotocol.wordpress.com/2011/09/15/chile-battles...
Epidemic Hazard in India on Saturday, 17 September, 2011 at 03:16 (03:16 AM) UTC.
| Description |
| The Department of Health and Family Welfare has informed that it had received a message through telephone on 12th September 2011 of an outbreak of fever of unknown cause leading to three deaths at Poilwa village, Peren District. Immediately the State Rapid Response Team (RRT) of Integrated Disease Surveillance Project (IDSP), Nagaland, comprising of Dr. John Kemp (State Surveillance Officer), Dr. Sao Tunyi (Epidemiologist), Dr. Kevisevolie Sekhose (Epidemiologist), and Venezo Vasa (Entomologist) conducted an outbreak investigation at Poilwa village. The team collected three samples from suspected cases out of which all the three were tested positive for Scrub Typhus. Till date, there are 9 cases with 3 deaths. This was stated in a official press note issued by Dr. Imtimeren Jamir, the Principal Director, Directorate of Health & Family Welfare, Kohima. Scrub Typhus is Rickettsial disease caused Orientia tsutsugamushi and transmitted by the bite of mite called Leptotrombidium deliense. In Nagaland, it was formerly detected by IDSP with Central Surveillance Team at Longsa village Mokokchung in 2006, and in Porba village of Phek District in 2007. The State RRT team carried out the outbreak investigation along with doing and entomological survey. The patients were treated with appropriate medicines and awareness and preventive measures were communicated with the villagers. The concerned local health authorities and programs are informed for further necessary action. The mop-up operation is being carried out by the National Vector Borne Disease Control Program. |
| Biohazard name: |
Typhus (Scrub) |
| Biohazard level: |
3/4 Hight |
| Biohazard desc.: |
Bacteria and viruses that can cause severe to fatal disease in humans, but for which vaccines or other treatments exist, such as anthrax, West Nile virus, Venezuelan equine encephalitis, SARS virus, variola virus (smallpox), tuberculosis, typhus, Rift Valley fever, Rocky Mountain spotted fever, yellow fever, and malaria. Among parasites Plasmodium falciparum, which causes Malaria, and Trypanosoma cruzi, which causes trypanosomiasis, also come under this level. |
| Symptoms: |
- After bite by infected mite larvae called chiggers, papule develops at the biting site which ulcerates and eventually heals with the development of a black eschar. - Patients develop sudden fever with headache, weakness, myalgia, generalized enlargement of lymph nodes, photophobia, and dry cough. - A week later, rash appears on the trunk, then on the extremities, and turns pale within a few days. - Symptoms generally disappear after two weeks even without treatment. - However, in severe cases with Pneumonia and Myocarditis, mortality may reach 30% Diagnosis - The most commonly used test for diagnosis is Wel-Felix Test, which is available at State IDSP laboratory, Kohima. - More specific serological tests like detection of IgM can also be done for diagnosis. |
| Status: |
confirmed
|
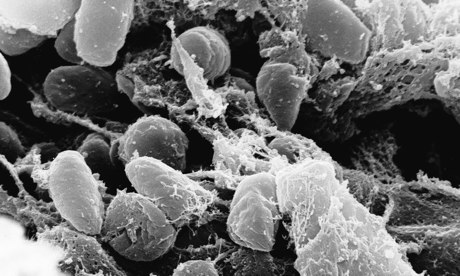
Turns out, the plague isn't just ancient history. New Mexico health officials recently confirmed the first human case of bubonic plague — previously known as the "Black Death" — to surface in the U.S. in 2011.
An unidentified 58-year-old man was hospitalized for a week after suffering from a high fever, pain in his abdomen and groin, and swollen lymph nodes, reports the New York Daily News. (Officials declined to say when the man was released from the hospital.) A blood sample from the man tested positive for the disease.
http://healthland.time.com/2011/05/10/first-case-of-bubonic-plague-...
Epidemic Hazard in USA on Saturday, 17 September, 2011 at 03:33 (03:33 AM) UTC.
| Description |
Umatilla County health officials today confirmed a case of plague in an adult male county resident. He may have been infected while hunting in Lake County, noted Sharon Waldern, clinic supervisor for the county’s public health department. “Lake County had two cases of human plague last year.” The man has been hospitalized and is receiving treatment, Waldern noted. “People need to realize he was never considered contagious and he started treatment fairly quickly.” Plague is spread to humans through a bite from an infected flea. The disease is serious but treatable with antibiotics if caught early, officials said. Plague can be passed from fleas feeding on infected rodents and then transmitted to humans. Direct contact with infected tissues or fluids from handling sick or dead animals can pass the disease, as well as through respiratory droplets from cats and humans with pneumonic plague, officials said in a press release. Some types are spread from person to person, but that is not the case here, Waldern said. Symptoms typically develop within one to four days and up to seven days after exposure and include fever, chills, headache, weakness and a bloody or watery cough due to pneumonia, enlarged, tender lymph nodes, abdominal pain and bleeding into the skin or other organs.
Plague is rare in Oregon. Only three human cases have been diagnosed since 1995 and they all recovered. Last year two human cases of plague were diagnosed in Lake County. As far as she knows, this is the first ever incident in Umatilla County. “In this recent case it is important to stay away from flea-infested areas and to recognize the symptoms. People can protect themselves, their family members and their pets,” said Genni Lehnert-Beers, administrator for Umatilla County Health Department. “Using flea treatment on your pets is very important, because your pets can bring fleas into your home.” People should contact their health care provider or veterinarian if plague is suspected. Early treatment for people and pets with appropriate antibiotics is essential to curing plague infections. Untreated plague can be fatal for animals and people. Antibiotics to prevent or treat plague should be used only under the direction of a health care provider. Additional steps to prevent flea bites include wearing insect repellent, tucking pant cuffs into socks when in areas heavily occupied by rodents, and avoiding contact with wildlife including rodents. |
| Biohazard name: |
Plague (Bubonic) |
| Biohazard level: |
4/4 Hazardous |
| Biohazard desc.: |
Viruses and bacteria that cause severe to fatal disease in humans, and for which vaccines or other treatments are not available, such as Bolivian and Argentine hemorrhagic fevers, H5N1(bird flu), Dengue hemorrhagic fever, Marburg virus, Ebola virus, hantaviruses, Lassa fever, Crimean-Congo hemorrhagic fever, and other hemorrhagic or unidentified diseases. When dealing with biological hazards at this level the use of a Hazmat suit and a self-contained oxygen supply is mandatory. The entrance and exit of a Level Four biolab will contain multiple showers, a vacuum room, an ultraviolet light room, autonomous detection system, and other safety precautions designed to destroy all traces of the biohazard. Multiple airlocks are employed and are electronically secured to prevent both doors opening at the same time. All air and water service going to and coming from a Biosafety Level 4 (P4) lab will undergo similar decontamination procedures to eliminate the possibility of an accidental release. |
| Symptoms: |
|
StatuThe Black Death: Bubonic Plague
|
confirmed
http://hisz.rsoe.hu/alertmap/site/?pageid=event_desc&edis_id=EH...
|





You need to be a member of Earth Changes and the Pole Shift to add comments!
Join Earth Changes and the Pole Shift