Disease outbreaks will increase as per ZetaTalk
Taking Sick
On Jan 15, 1998 ZetaTalk stated that Illness will increase as Planet X approaches. Zetas right again !!!
- ZetaTalk: Take Sick, written Feb 15, 1998.
- Increasingly, as the pole shift nears, the populace will take sick. This will take the form of known illnesses occurring more frequently, seemingly depressed immune systems, but will also appear as new and puzzling illnesses not seen before in the memory of man. What is going on here?
The changes at the core of the Earth that have resulted in El Nino weather patterns and white buffalo and deformed frogs also affect man. The germs are on the move. Their carriers are on the move. And thus humans are exposed to diseases that are so rare as to be undocumented in medical journals.
You will see increasing illness, odd illnesses, microbes that travel because an insect is scattering about and spreading germs in places where it normally doesn't travel. 90% of all the illness and distress you're going to see is a natural situation, a natural occurrence. Because of the changing, swirling in the core of the Earth, and this will continue to up-tick until the pole shift.
And reiterated in 1999
- ZetaTalk: Next 3 1/2 Years, written Sep 15, 1999.
- Sickness will slightly increase from where it is today. There is a lot of illness now because people who are already unstable are unable to take the turmoil caused by the increased emanations from the Earth. Some of them have simply sensed what is coming and have decided to die. This is true of animals as well as humans. Sickness will increase, but not to the point where it is going to get exponentially worse.
On Feb 2, 2000 a Washington report confirmed this increase, and published concerns were subsequently reported.
- Diseases From Around World Threatening U.S.
Reuters, Feb 2, 2000 - 30 New Diseases Make Global Debut
At least 30 previously unknown diseases have appeared globally since 1973, including HIV, AIDS, Hepatitis C, Ebola haemorrhagic fever and the encephalitis-related Nipah virus that emerged in Indonesia. Twenty well-known infectious diseases such as tuberculosis, malaria, and cholera have re-emerged or spread since 1973. - Is Global Warming Harmful to Health?
Scientific American, August 2000 - Notably, computer models predict that global warming, and other climate alterations it induces, will expand the incidence and distribution of many serious medical disorders. Disturbingly, these forecasts seem to be coming true.
And since this time, SARS and increased incidence of flesh eating disease,
and entire cruise ships regularly returning to port with the passengers ill with stomach flu have been reported.
Depressed immune systems?
Zetas RIGHT Again!
After the pole shift, there will be many opportunistic diseases that will afflict mankind. This does not require an imagination, as today they afflict mankind after disasters. The primary affliction will be from sewage laden water, which will pollute the drinking water man is forced to use. We have been adamant about mankind distilling their drinking water after the pole shift for this reason. Distillation removes heavy metals as well as killing microbes by the boiling process. Any disease that flourishes in malnourished bodies and in areas of poor hygiene will take advantage of the pole shift disasters. Scurvy due to lack of Vitamin C will occur, with bleeding gums and even death if not corrected. Many weeds are high in Vitamin C and survivors should arm themselves with knowledge about the vitamin content of weeds. Unprotected sex by survivors either taking advantage of the weak, as in rape, or by simple distraction and grief and a lack of contraceptive devices will spread AIDS and hepatitis. Morgellons, which is caused by a synergy of parasites and microbes when the immune system is low will likely increase. There will be outbreaks of diseases which were endemic in the past, such as small pox or measles, but in those survivor communities where the members have been immunized in the past these will be limited and quarantines can help in this regard.
http://www.zetatalk5.com/ning/20no2010.htm
Chile battles youth unrest and typhoid fever outbreak
 September 15, 2011 – SANTIAGO – Chile’s problems dealing with youth unrest over slow education reforms are being compounded by concerns the capital may be in the grip of a typhoid fever outbreak. The government has battled to enforce restraint on law enforcement agencies amid angry student-led protests, which have disrupted urban centers across the country for more than a month. The reforms demanded by youth groups are nowhere near being implemented and protests continue to simmer with support from teachers and workers unions. Now authorities are faced with the more immediate risk of typhoid. Health authorities issued repeated alerts for tougher hygiene checks and controls after they found several people infected and seriously ill with typhoid in the western metropolitan area of Santiago. At least seven cases were confirmed by the Public Health Institute but there were no immediate reports of fatalities. “Typhoid fever is an acute infectious disease triggered by a salmonella bacteria strain,” Institute Director Maria Teresa Valenzuela said. In most cases the infection is caused by consumption of contaminated food and drink or fruit and vegetables grown in areas where contaminated water is used in irrigation. Typhoid fever produces symptoms of high fever, diarrhea or intense headaches. The Santiago region has been prone to typhoid outbreaks since the 1990s when incidence of the disease caused up to 190 cases a year.
September 15, 2011 – SANTIAGO – Chile’s problems dealing with youth unrest over slow education reforms are being compounded by concerns the capital may be in the grip of a typhoid fever outbreak. The government has battled to enforce restraint on law enforcement agencies amid angry student-led protests, which have disrupted urban centers across the country for more than a month. The reforms demanded by youth groups are nowhere near being implemented and protests continue to simmer with support from teachers and workers unions. Now authorities are faced with the more immediate risk of typhoid. Health authorities issued repeated alerts for tougher hygiene checks and controls after they found several people infected and seriously ill with typhoid in the western metropolitan area of Santiago. At least seven cases were confirmed by the Public Health Institute but there were no immediate reports of fatalities. “Typhoid fever is an acute infectious disease triggered by a salmonella bacteria strain,” Institute Director Maria Teresa Valenzuela said. In most cases the infection is caused by consumption of contaminated food and drink or fruit and vegetables grown in areas where contaminated water is used in irrigation. Typhoid fever produces symptoms of high fever, diarrhea or intense headaches. The Santiago region has been prone to typhoid outbreaks since the 1990s when incidence of the disease caused up to 190 cases a year.
http://theextinctionprotocol.wordpress.com/2011/09/15/chile-battles...
Epidemic Hazard in India on Saturday, 17 September, 2011 at 03:16 (03:16 AM) UTC.
| Description | |
| The Department of Health and Family Welfare has informed that it had received a message through telephone on 12th September 2011 of an outbreak of fever of unknown cause leading to three deaths at Poilwa village, Peren District. Immediately the State Rapid Response Team (RRT) of Integrated Disease Surveillance Project (IDSP), Nagaland, comprising of Dr. John Kemp (State Surveillance Officer), Dr. Sao Tunyi (Epidemiologist), Dr. Kevisevolie Sekhose (Epidemiologist), and Venezo Vasa (Entomologist) conducted an outbreak investigation at Poilwa village. The team collected three samples from suspected cases out of which all the three were tested positive for Scrub Typhus. Till date, there are 9 cases with 3 deaths. This was stated in a official press note issued by Dr. Imtimeren Jamir, the Principal Director, Directorate of Health & Family Welfare, Kohima. Scrub Typhus is Rickettsial disease caused Orientia tsutsugamushi and transmitted by the bite of mite called Leptotrombidium deliense. In Nagaland, it was formerly detected by IDSP with Central Surveillance Team at Longsa village Mokokchung in 2006, and in Porba village of Phek District in 2007. The State RRT team carried out the outbreak investigation along with doing and entomological survey. The patients were treated with appropriate medicines and awareness and preventive measures were communicated with the villagers. The concerned local health authorities and programs are informed for further necessary action. The mop-up operation is being carried out by the National Vector Borne Disease Control Program. | |
| Biohazard name: | Typhus (Scrub) |
| Biohazard level: | 3/4 Hight |
| Biohazard desc.: | Bacteria and viruses that can cause severe to fatal disease in humans, but for which vaccines or other treatments exist, such as anthrax, West Nile virus, Venezuelan equine encephalitis, SARS virus, variola virus (smallpox), tuberculosis, typhus, Rift Valley fever, Rocky Mountain spotted fever, yellow fever, and malaria. Among parasites Plasmodium falciparum, which causes Malaria, and Trypanosoma cruzi, which causes trypanosomiasis, also come under this level. |
| Symptoms: | - After bite by infected mite larvae called chiggers, papule develops at the biting site which ulcerates and eventually heals with the development of a black eschar. - Patients develop sudden fever with headache, weakness, myalgia, generalized enlargement of lymph nodes, photophobia, and dry cough. - A week later, rash appears on the trunk, then on the extremities, and turns pale within a few days. - Symptoms generally disappear after two weeks even without treatment. - However, in severe cases with Pneumonia and Myocarditis, mortality may reach 30% Diagnosis - The most commonly used test for diagnosis is Wel-Felix Test, which is available at State IDSP laboratory, Kohima. - More specific serological tests like detection of IgM can also be done for diagnosis. |
| Status: | confirmed
|
Turns out, the plague isn't just ancient history. New Mexico health officials recently confirmed the first human case of bubonic plague — previously known as the "Black Death" — to surface in the U.S. in 2011.
An unidentified 58-year-old man was hospitalized for a week after suffering from a high fever, pain in his abdomen and groin, and swollen lymph nodes, reports the New York Daily News. (Officials declined to say when the man was released from the hospital.) A blood sample from the man tested positive for the disease.
http://healthland.time.com/2011/05/10/first-case-of-bubonic-plague-...
Epidemic Hazard in USA on Saturday, 17 September, 2011 at 03:33 (03:33 AM) UTC.
| Description | |
| Umatilla County health officials today confirmed a case of plague in an adult male county resident. He may have been infected while hunting in Lake County, noted Sharon Waldern, clinic supervisor for the county’s public health department. “Lake County had two cases of human plague last year.” The man has been hospitalized and is receiving treatment, Waldern noted. “People need to realize he was never considered contagious and he started treatment fairly quickly.” Plague is spread to humans through a bite from an infected flea. The disease is serious but treatable with antibiotics if caught early, officials said. Plague can be passed from fleas feeding on infected rodents and then transmitted to humans. Direct contact with infected tissues or fluids from handling sick or dead animals can pass the disease, as well as through respiratory droplets from cats and humans with pneumonic plague, officials said in a press release. Some types are spread from person to person, but that is not the case here, Waldern said. Symptoms typically develop within one to four days and up to seven days after exposure and include fever, chills, headache, weakness and a bloody or watery cough due to pneumonia, enlarged, tender lymph nodes, abdominal pain and bleeding into the skin or other organs. Plague is rare in Oregon. Only three human cases have been diagnosed since 1995 and they all recovered. Last year two human cases of plague were diagnosed in Lake County. As far as she knows, this is the first ever incident in Umatilla County. “In this recent case it is important to stay away from flea-infested areas and to recognize the symptoms. People can protect themselves, their family members and their pets,” said Genni Lehnert-Beers, administrator for Umatilla County Health Department. “Using flea treatment on your pets is very important, because your pets can bring fleas into your home.” People should contact their health care provider or veterinarian if plague is suspected. Early treatment for people and pets with appropriate antibiotics is essential to curing plague infections. Untreated plague can be fatal for animals and people. Antibiotics to prevent or treat plague should be used only under the direction of a health care provider. Additional steps to prevent flea bites include wearing insect repellent, tucking pant cuffs into socks when in areas heavily occupied by rodents, and avoiding contact with wildlife including rodents. |
|
| Biohazard name: | Plague (Bubonic) |
| Biohazard level: | 4/4 Hazardous |
| Biohazard desc.: | Viruses and bacteria that cause severe to fatal disease in humans, and for which vaccines or other treatments are not available, such as Bolivian and Argentine hemorrhagic fevers, H5N1(bird flu), Dengue hemorrhagic fever, Marburg virus, Ebola virus, hantaviruses, Lassa fever, Crimean-Congo hemorrhagic fever, and other hemorrhagic or unidentified diseases. When dealing with biological hazards at this level the use of a Hazmat suit and a self-contained oxygen supply is mandatory. The entrance and exit of a Level Four biolab will contain multiple showers, a vacuum room, an ultraviolet light room, autonomous detection system, and other safety precautions designed to destroy all traces of the biohazard. Multiple airlocks are employed and are electronically secured to prevent both doors opening at the same time. All air and water service going to and coming from a Biosafety Level 4 (P4) lab will undergo similar decontamination procedures to eliminate the possibility of an accidental release. |
| Symptoms: | |
StatuThe Black Death: Bubonic Plague
|
confirmed http://hisz.rsoe.hu/alertmap/site/?pageid=event_desc&edis_id=EH...
|
Comment
-
Comment by Howard on August 30, 2012 at 8:35pm
-
Mysterious New 'Heartland Virus' Discovered In Missouri (August 30) -
http://www.npr.org/blogs/health/2012/08/29/160272241/mysterious-new...
Two Missouri farmers have been infected with a brand-new tick-borne virus that the Centers for Disease Control and Prevention is calling the Heartland virus.
The men recovered but suffered serious illness that required hospital care and weeks of convalescence. Symptoms included fever, severe fatigue, headache and nausea. Their platelet counts plummeted, but even though platelets are necessary for blood clotting, the men didn't suffer abnormal bleeding.
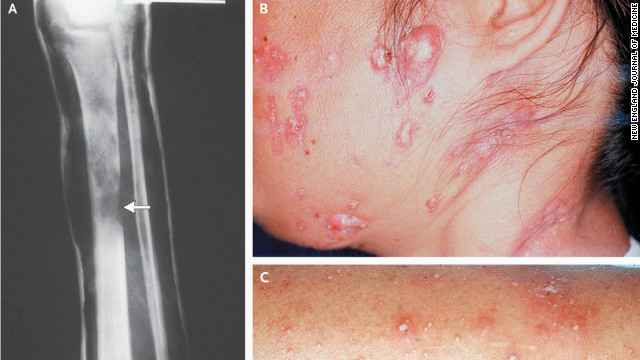
A report on the new virus is in the current issue of the New England Journal of Medicine.
So far, the Missouri men are the only known cases of Heartland virus in the world. But experts are sure they'll find more.
After all, the men lived 60 miles apart and got infected independently. That means there must be more of the mysterious new virus in the northwest Missouri environment.
"We expect to find new cases," Dr. William Nicholson of the CDC told Shots. "We expect this thing may be wider in geographic distribution than we currently know."
The virus is dubbed "Heartland" not only because that's where it was discovered, but because of who found it: an astute infectious disease doctor named Scott Folk who works at Heartland Regional Medical Center in St. Joseph, Mo.
Folk is well-known to the CDC. "Whenever he sends us a sample, we pay attention because we're likely to find something," Nicholson says. In this case, Folk sent samples from 14 patients back in 2009.
Two of them puzzled the CDC experts — and then surprised them when electron microscope studies revealed a novel virus now called Heartland. The other dozen cases involved a more common tick-borne bacterial infection called ehrlichiosis.
"We're pretty excited about it," Nicholson says about the Heartland virus. "It's not every day that you find something new — particularly in the world of tick-borne diseases. We often work with what might be considered antique diseases, such as Rocky Mountain spotted fever."
Nicholson says the new virus is in the phlebovirus family, which contains more than 70 members. And here's another twist: Heartland virus appears to be a cousin of another new human virus called severe fever with thrombocytopenia syndrome virus, discovered last year in China. Another possible cousin may be Bhanja virus, a little-studied virus that has been found in some mammals, birds and reptiles in Asia, Africa and Europe.
Nicholson says the CDC, working with Folk, is looking for other people with symptoms similar to the two Heartland victims to see if they're infected with the same virus. The researchers are also analyzing thousands of samples from Missouri ticks, other crawling insects, and animals wild and domestic to see if any harbor Heartland virus.
-
Comment by Robyn Appleton on August 25, 2012 at 6:30am
-
EDIS Number: EP-20120720-35859-SLE
Event type: Epidemic
Date/Time: Friday, 20 July, 2012 at 18:20 (06:20 PM) UTC
Continent: Africa
Country: Sierra Leone
County / State: Northern Province
Area: Port Loko, Kambia, Pujehun and Kailahun districts
Coordinate: N 8° 46.000, W 12° 47.250
Dead person(s): 258
Infected person(s): 13 000
Updated: Friday, 24 August, 2012 at 06:08 UTC
Description;
Sierra Leone's health ministry said Thursday that deaths from a cholera outbreak had reached 220, affecting over 12,000 people in the west African nation, which is struggling to curb the disease. "Some 12,140 people are affected nationwide in 10 of 12 districts," the health ministry's director of disease prevention and control, Amara Jambai, told journalists, saying the figure included cases recorded up to Wednesday. This is two more districts than were reported last week when the death toll stood at 176, prompting President Ernest Koroma to declare the outbreak a "public health emergency". "The outbreak has peaked mainly in slum areas in the capital due to poor sanitation including areas without latrines or people drinking contaminated water," Jambai said. International health organisations are grappling to stem the spread of the outbreak which has also hit neighbouring Guinea. Jambai said the outbreak had "opened up a window of opportunity whereby our partners are providing resources in a faster and more coherent manner."
He said cholera cases were expected to rise in September as the country's annual rainy season reaches its peak. According to the World Health Organisation (WHO) representative in Freetown, Wondimagenehu Alemu: "Everywhere is at risk but everything is being done combat the spread." Amanda McClelland of the International Federation of Red Cross last week said the outbreak had the potential to be "devastating" and was proving difficult to control. The water-borne disease has also hit Mali and Niger, as well as Sierra Leone's northern neighbour Guinea, killing 82 people in that country since February. Poor water and sanitation systems give rise to the disease, an acute intestinal infection caused by ingesting contaminated food and water which causes acute diarrhoea and vomiting and can kill in hours, according to the WHO.
-
Comment by lonne rey on August 24, 2012 at 7:51pm
-
Researchers identify rare adult immune disease in Asia
Doctors have identified the disease as a syndrome that creates AIDS-like symptoms but say it’s not a virus, and it’s not contagious.
-
Comment by Robyn Appleton on August 16, 2012 at 1:44am
-
EDIS Number: BH-20120815-36186-USA
Event type: Biological Hazard
Date/Time: Wednesday, 15 August, 2012 at 03:14 (03:14 AM) UTC
Continent: North-America
Country: USA
County / State: State of Texas
Area: Dallas County
Coordinate: N 32° 48.148, W 96° 50.106
Dead person(s): 9
Infected person(s): 175
Description;
Nine people have died from a West Nile virus outbreak that infected 175 people in Dallas County, Texas, prompting officials to declare a state of emergency. The emergency was declared on Friday by Dallas County Judge Clay Jenkins, the county’s director of homeland security and emergency management. “This declaration will expand our avenues DisasterNew assistance in our ongoing battle with West Nile virus,” Jenkins said. “While we are busy doing everything we can to keep residents well informed and as protected as possible, we need your help.” Jenkins also said that planes would be spraying insecticide over areas most effected by the virus, which is spread by mosquitoes. He assured citizens that the insecticide is safe and that the planes will be precise in their spraying. Tarrant County has also received 146 reported cases of West Nile in the last few weeks. The county has not declared a state of emergency, though. Houston officials are warning residents of an increased threat of the virus. “Houston can definitely expect an increase in West Nile disease,” said Kristy Murray, an infectious disease specialist at the Baylor College of Medicine’s National School of Tropical Medicine, DisasterNews reports. “From mid-August through September is the big season here.”
Biohazard name: West Nile virus outbreak
Biohazard level: 2/4 Medium
Source.
-
Comment by Robyn Appleton on August 9, 2012 at 3:44am
-
EDIS Number: EP-20120808-36093-PAK
Event type: Epidemic
Date/Time: Wednesday, 08 August, 2012 at 04:48 (04:48 AM) UTC
Continent: Asia
Country: Pakistan
County / State: North West Frontier Province
Area: Swabi District
Coordinate: N 34° 7.000, E 72° 28.000
Infected person(s): 130
Description
Around 130 people suffering from cholera and gastroenteritis in Swabi district’s Takeel village were rushed to tehsil and district headquarters (DHQ) hospitals on Tuesday. According to Executive District Officer (EDO) Dr Gul Muhammad Khan, the victims had been drinking water from a contaminated spring in the area, leading to the outbreak. He added that the area was a remote village in Gadoon, where people lack healthcare and educational facilities. Gul said the district health department has dispatched a medical mobile unit along with an ambulance to contain the outbreak. He maintained it was the responsibility of basic health units (BHU) in Ghani Chatra and Ghabasini – the village’s adjacent areas – but they have not been provided a staff by the government yet. “If the BHUs had staff, the number of people we had to vaccinate would have been less,” he added. Mukhtiar Khan, an administrative official in Topi’s Tehsil Headquarters Hospital said more than 35 cholera patients had been admitted so far. “We vaccinate the victims, try to control their dehydration… if their condition is serious, they are transferred to the DHQ hospital,” he informed. The official added that despite lacking in facilities, they were extending all possible medical care to the patients.Biohazard name: Cholerae Outbreak
Biohazard level: 2/4 Medium
-
Comment by Robyn Appleton on August 7, 2012 at 5:59pm
-
EDIS Number: EH-20120728-35961-ZWE
Event type: Epidemic Hazard
Date/Time: Saturday, 28 July, 2012 at 03:34 (03:34 AM) UTC
Continent: Africa
Country: Zimbabwe
County / State: Multiple areas
Area: Harare (Capital City) and Chitungwiza
Coordinate: S 18° 0.000, E 31° 3.000
Infected person(s): 111
Updated: Thursday, 02 August, 2012 at 13:56 UTC
Description
A typhoid outbreak has hit Harare and Chitungwiza, with at least 111 confirmed cases by yesterday. City officials attributed the outbreak to water shortages in the city and its satellite towns of Chitungwiza, Norton, Ruwa and Epworth. Typhoid fever, also known as typhoid, is a common worldwide bacterial disease, transmitted by the ingestion of food or water contaminated with the faeces of an infected person. Chitungwiza, Norton, Ruwa and Epworth receive water from Harare whose water treatment plant is facing mechanical problems. The majority of the cases are in Chitungwiza where at least 83 people were treated for the disease. Harare had 28 confirmed cases, with 25 of them occurring at a supermarket in the Avenues area, while three were in Mabvuku/Tafara suburb. City health services director Dr Prosper Chonzi said the supermarket has since been barred from selling fresh, raw and cooked foods.
"We are still tracing the customers who bought food from the supermarket," he said. "We have a full outbreak response team in Mabvuku and Tafara. We have stationed a doctor at Mabvuku clinic to attend to the cases." Dr Chonzi said six of the affected people were detained at the Beatrice Infectious Diseases Hospital. He said the majority of the cases were treated and discharged depending on the severity of their conditions. The outbreak in Tafara and Mabvuku, Dr Chonzi said, was caused by the use of unprotected wells. He said the outbreak in Chitungwiza was posing serious threats to Harare because of the high human traffic between the two urban centres. Chitungwiza acting director of health services Mr Herbert Chiroodza said they would drill boreholes in the affected areas. "We did alert Harare City Council and the Ministry of Health and Child Welfare on the outbreak," he said. "We have since made negotiations with Harare so that the affected areas do not experience water cuts during this outbreak."
Chitungwiza residents urged the authorities to address the water situation before the disease gets worse. The residents believe that a death which occurred in the location was linked to the outbreak and that people who attended the man's burial could have contracted and passed on the disease. "We used to get tap water thrice a week, but now we are getting it only once a week. Can you imagine that we last had supplies on Saturday and we do not know when we are going to have tap water," said Mrs Kudzanai Joseph. She said residents have no choice, but to dig shallow wells at their homes. Another resident, Ms Nyasha Kujeke, who is still recuperating from typhoid, said the municipality must act urgently on the disease.
"Everyone is sick in this area. We do not know where else to get safe drinking water," she said. "The boreholes are overwhelmed, our wells are contaminated. Should we buy bottled water while we are paying water bills to council?" Harare town clerk Dr Tendai Mahachi said on Tuesday that most of Harare would not have adequate water because of the mechanical problems. The water problems have been traced to Norton, which is accused of discharging 10 million litres of raw sewer close to Harare's raw water abstraction point. Norton chief executive officer Mr Winslow Muyambi confirmed his council was discharging raw sewer into Lake Manyame.
Source; http://hisz.rsoe.hu/alertmap/site/?pageid=event_summary&edis_id...
-
Comment by Robyn Appleton on August 2, 2012 at 3:03pm
-
Epidemic Hazard in Uganda on Thursday, 26 July, 2012 at 15:57 (03:57 PM) UTC.
EDIS Number:
EH-20120726-35941-UGA
Event type:
Epidemic Hazard
Date/Time:
Thursday, 26 July, 2012 at 15:57 (03:57 PM) UTC
Continent:
Africa
Country:
Uganda
County / State:
Western Uganda
Area:
Kibaale District, Mbarara and the Capital City (Kampala)
Coordinate:
N 0° 46.419, E 31° 4.590
Foreign people:
Affected is unknown.
Dead person(s):
18
Infected person(s):
36
Sixteen people are reported dead in Uganda from a mystery illness. The Uganda publication UG Pulse reports that a strange illness, cause unknown, is spreading in the Kibaale district in western Uganda. The District Health Officer, Dr. Dan Kyamanwa, stated that 11 of the deaths were from the same family in the Nyamarunda Sub County. A twelfth death was a health officer. There are also reports of the illness appearing in the clinical officer who treated the family from Nyamarunda and a driver who transported the deceased. Kyamanwa says that symptoms of the illness include high fever, vomiting, diarrhea and systems failure. Death occurs within four to seven days.The Ugandan government is reportedly sending a team of experts to investigate the outbreak.
Biohazard name: Unidentified fatal disease
Biohazard level: 4/4 Hazardous
Update; Saturday, 28 July, 2012 at 13:38 UTC
The deadly Ebola virus has killed 14 people in western Uganda this month, Ugandan health officials said on Saturday, ending weeks of speculation about the cause of a strange disease that had many people fleeing their homes. The officials and a World Health Organization representative told a news conference in Kampala Saturday that there is "an outbreak of Ebola" in Uganda. "Laboratory investigations done at the Uganda Virus Research Institute…have confirmed that the strange disease reported in Kibaale is indeed Ebola hemorrhagic fever," the Ugandan government and WHO said in joint statement. Kibaale is a district in mid-western Uganda, where people in recent weeks have been troubled by a mysterious illness that seemed to have come from nowhere. Ugandan health officials had been stumped as well, and spent weeks conducting laboratory tests that were at first inconclusive. On Friday, Joaquim Saweka, the WHO representative in Uganda, told The Associated Press that investigators were "not so sure" it was Ebola, and a Ugandan health official dismissed the possibility of Ebola as merely a rumor. It appears firm evidence of Ebola was clinched overnight.
Health officials told reporters in Kampala that the 14 dead were among 20 reported with the disease. Two of the infected have been isolated for examination by researchers and health officials. A clinical officer and, days later, her 4-month-old baby died from the disease caused by the Ebola virus, officials said. The officials urged Ugandans to be calm, saying a national emergency taskforce had been set up to stop the disease from spreading far and wide. There is no cure or vaccine for Ebola, and in Uganda, where in 2000 the disease killed 224 people and left hundreds more traumatized, it resurrects terrible memories. Ebola, which manifests itself as a hemorrhagic fever, is highly infectious and kills quickly. It was first reported in 1976 in Congo and is named for the river where it was recognized, according to the Centers for Disease Control and Prevention. Scientists don't know the natural reservoir of the virus, but they suspect the first victim in an Ebola outbreak gets infected through contact with an infected animal, such as a monkey. The virus can be transmitted in several ways, including through direct contact with the blood of an infected person. During communal funerals, for example, when the bereaved come into contact with an Ebola victim, the virus can be contracted, officials said, warning against unnecessary contact with suspected cases of Ebola.Update; Monday, 30 July, 2012 at 04:48 UTC
Ugandan authorities did not initially detect an Ebola outbreak because patients weren't showing typical symptoms of the lethal virus, the nation's health minister reported on Sunday. Patients had fevers and were vomiting, but did not show other typical symptoms like hemorrhaging, Health Minister Dr. Christine Ondoa said. A team made up of personnel from the Centers for Disease Control and Prevention, the Ugandan health ministry and the World Health Organization early Monday were in Kibaale, a district in the midwestern part of the landlocked central African nation, WHO said in a statement. Medecins Sans Frontieres, also known as Doctors Without Borders, also is involved in setting up an "isolation center" at Kibaale's hospital. National health authorities say the outbreak has infected at least 20 people, of whom 14 have died. Nine of the deaths were from a single household in the village of Nyanswiga, according to WHO. A medic who was treating victims is among the dead, Ondoa said. Officials are trying to determine the extent of the outbreak, CDC spokesman Tom Skinner said Sunday. The Atlanta-based organization was sending about five people to join a group of CDC staffers who are permanently based in Uganda, according to the spokesman.
"These outbreaks have a tendency to stamp themselves out, if you will, if we can get in and ... stop the chain of transmission," he said. Ondoa described the Ebola-Sudan strain detected as "mild" compared to other types of Ebola, noting that victims' lives can be saved with intervention. The cases have emerged in Kibaale, where a national task force had been mobilized in an effort to combat the outbreak. As of early Monday in Uganda, two people with the virus remained hospitalized in stable condition, said WHO. One was a 38-year-old woman who'd attended to her sister, the medic who died, and another was a 30-year-old woman who participated in the burial of one of the other victims. The Ebola virus is considered a highly infectious disease spread through direct contact with bodily fluids, with symptoms that include fever, vomiting, diarrhea, abdominal pain, headache, measles-like rash, red eyes and at times bleeding from body openings. Health officials urged the public to report suspected cases and avoid contact with anyone who has contracted the virus and to disinfect the bedding and clothing of an infected person by using protective gloves and masks. Officials also advised against eating dead animals, especially monkeys, and to avoid public gatherings in the affected district. Given these precautions, WHO said in its statement that it would not recommend any travel restrictions to Uganda because of the Ebola outbreak.Update; Monday, 30 July, 2012 at 18:37 UTC
Ebola, one of the world’s deadliest viruses, has been confirmed in Uganda, where 14 people have already died from what health officials were calling a mysterious illness. The illness was not immediately described as Ebola because patients were not showing the typical signs of the lethal disease, the nation’s health minister told CNN on Sunday. After news of the virus broke, a team of health experts from the Centers for Disease Control and Prevention (CDC), the World Health Organization (WHO) and the Ugandan government were deployed to the area to begin emergency response measures, according to a government statement. The experts discovered the strain was Ebola Sudan, one of the most common strains of the virus. This particular strain has been associated with a 70 percent mortality rate in recent years. The virus manifests as a hemorrhagic fever. The last severe outbreak occurred in 2000, killing 224 people in Uganda. It was first reported in 1976 in what is now the Democratic Republic of Congo, according to the CDC. The strange disease was first reported in the area several weeks ago, according to a government statement.
Ignatius Besisira, an MP for Buyaga East County in the Kibaale district, said people first believed the unexplained deaths were from witchcraft. “Immediately, when there was confirmation that it was Ebola … patients ran out of Kagadi hospital (where some of the victims had died),” Besisira told the Guardian. “Even the medical officers are very, very frightened.” Lab tests confirmed the illness was Ebola hemorrhagic fever. A baby from the village of Nyanswiga was the first confirmed death and so far 14 of some 20 that are known to have been infected have died. A clinical officer who treated the original case also fell ill and died soon afterward. Her four-month-old baby, admitted for treatment last Monday, died four days later. The clinical officer’s sister, who took care of the baby when she became ill, has been admitted for treatment with similar symptoms, but is currently in stable condition, the government statement said. There is no treatment or vaccine against Ebola, which is transmitted through close contact and, depending on the strain, can kill up to 90 percent of those who contract the virus. While Ebola outbreaks occur every few years, the virus’s delicate composition has so far impeded a significant, long-duration attack. But much about the disease remains a mystery.
The CDC has a team of scientists stationed at a Ugandan laboratory who study Ebola and other deadly viruses that are often found in equatorial Africa. Ebola is among a list of viruses highlighted by the US as a potential biological-weapons threat. Officials are currently trying to determine the extent of the outbreak, CDC spokesman Tom Skinner told CNN.com on Sunday. “These outbreaks have a tendency to stamp themselves out, if you will, if we can get in and … stop the chain of transmission,” he explained. Health officials are urging area residents to report any suspected cases and avoid contact with anyone who has contracted the virus and to disinfect bedding and clothing of an infected person by using protective gloves and masks. They also advise against eating dead animals, especially monkeys, and to avoid public gatherings if at all possible. Despite the ongoing threat, the WHO said in its statement that it does not recommend travel restrictions to Uganda because of the outbreak. Besisira said officials in Kibaale had released radio broadcasts outlining the precautionary measures on Saturday. “We have assured (the people) that we have a very strong team … who are making sure the disease is controlled … I am very confident we can contain it,” he added. While there are no reports of people moving out of the region, the Daily Nation newspaper in Kenya said on Sunday that people were leaving the area around Kagadi town, where the disease first appeared. “We have to move to safer places because we can easily get infected by this disease here,” the paper quoted a resident, Omuhereza Kugonza, as saying. Ebola is transmitted by direct contact with the body fluids and tissues of infected persons. It can also be transmitted by handling sick or dead infected wild animals, such as chimpanzees, gorillas, monkeys, forest antelope and fruit bats. Symptoms include sudden fever, intense weakness, muscle pain, headache and sore throat, followed by vomiting, diarrhea, rashes, impaired kidney and liver function and bleeding.Update; Tuesday, 31 July, 2012 at 11:53 UTC
Six more patients thought to have the highly infectious Ebola virus have been hospitalized in Uganda, days after investigators confirmed an outbreak of the disease in a remote Western corner of the country, a health official said on Monday. Stephen Byaruhanga, health secretary of the affected Kibaale district, said possible cases of Ebola, at first concentrated in a single village, are now being reported in more villages. "It's no longer just one village. There are many villages affected," Byaruhanga said. In a national address Monday, Uganda's president advised against unnecessary contact among people, saying suspected cases of Ebola should be reported immediately to health officials. Officials from Uganda's Ministry of Health and the World Health Organization announced on Saturday that the deadly Ebola virus killed 14 Ugandans this month, ending weeks of speculation about the cause of a strange illness that had some people fleeing their homes in the absence of reliable answers.
The deceased include a clinical officer who attended to a patient, and her four month-old child. Nine of the 14 deaths have occurred in a single household, the World Health Organization said Sunday. Ebola, which manifests itself as a hemorrhagic fever, is a potentially lethal disease that kills quickly. It was first reported in 1976 in Congo and is named for the river where it was recognized. According to the Centers for Disease Control and Prevention, Ebola is characterized by fever, headache, joint and muscle aches, sore throat, and weakness, followed by diarrhea, vomiting, and stomach pain. A rash, red eyes, hiccups and internal and external bleeding may be seen in some patients. If the six new cases are confirmed as Ebola, it would bring to 26 the number of Ugandans infected with Ebola. This is the fourth occurrence of Ebola in Uganda since 2000, when the disease killed 224 people and left hundreds more traumatized in northern Uganda. At least 42 people were killed in another outbreak in 2007, and there was a lone Ebola case in 2011.
Investigators took nearly a month to confirm Ebola's presence in Uganda this year. In Kibaale, a district with 600,000 residents, some villagers started abandoning their homes to escape what they thought was an illness caused by bad luck. One family lost nine members, and a clinical officer and her 4-month-old baby died from Ebola, Byaruhanga said. D.K. Lwamafa, of Uganda's Ministry of Health, told reporters on Saturday that one Ebola patient from Kibaale had been referred to the national hospital in the capital but had then died in Kibaale. The confirmation of Ebola's presence in the area has spread anxiety among sick villagers, who are refusing to go the hospital for fear they don't have Ebola and will contract it there. All suspected Ebola patients have been isolated at one hospital where patients admitted with other illnesses fled after Ebola was announced. Only the hospital's maternity ward still has patients, officials said, highlighting the deadly reputation of Ebola in a country where the authorities do not always respond quickly and effectively to emergencies and disasters.
Barnabas Tinkasimire, a lawmaker from the area, said that some nurses refused to look after Ebola patients after one clinical officer died and another was taken ill. "They are saying, `We can't remain here if there is no sufficient allowance,'" Tinkasimire said of medical officers handling Ebola cases. The lawmaker said the government's response so far has been poor and that it would have been worse without the technical support of organizations such as the World Health Organization and the U.S. Centers for Disease Control and Prevention. "It took long for the government to respond, and up to now many people don't know how to guard against Ebola. We need sensitization," he said. Scientists don't know the natural reservoir of the virus, but they suspect the first victim in an Ebola outbreak gets infected through contact with an infected animal. Some people are able to recover from Ebola and others are not for reasons not understood, however, it is known that patients who die usually have not developed a significant immune response to the virus at the time of death. The virus can be transmitted through direct contact with the blood or secretions of an infected person, or objects that have been contaminated with infected secretions. During communal funerals, for example, when the bereaved come into contact with an Ebola victim, the virus can be contracted, health officials said.Update; Wednesday, 01 August, 2012 at 02:58 UTC
Four more patients suspected to be suffering from Ebola have died as 14 new cases are also currently isolated in wards at Kagadi and Mulago hospitals. This brings the death toll to 18 in the country's third massive wave of Ebola outbreaks in the last one decade. Medical authorities were also Tuesday investigating a suspected Ebola case in Mbarara. The case was placed under isolation. The patients who died on Monday all from Kibaale were identified as Susan Nabulya from Burunzi village, the first patient to be admitted at Kagadi hospital, five-year-old Nicholas Asingwire (Kenga village), 12-year-old Kato (Nyamarunda village) and Frediano Nsabimaana of Nyamugusa village in Bwamiramira sub-county. Another 11 new suspected Ebola patients were Tuesday admitted at Kagadi hospital in Kibaale and three others in Mulago hospital in Kampala.
The number of suspected cases at Kagadi hospital has reached 18, which puts the total suspected cases at Kagadi and Mulago to 21. The three admitted in Mulago are also from Kibaale district; a four-year old boy, his mother and uncle, according to the deputy executive director, Dr. Doreen Male. However, the health ministry in a statement issued Tuesday said there were 18 patients in Kagadi hospital, of whom three are confirmed to have contracted Ebola. The health ministry's surveillance team in Kibaale, according to the statement, is, "actively and closely monitoring 40 people who are suspected to have got in contact with the dead." "These contacts have not shown any signs of the disease but will be monitored for 21 days," said the statement, adding that after 21 days, they will be declared Ebola-free if no signs are detected.
Kibaale district health officer, Dr. Dan Kyamanywa said that the new suspected Ebola patients were picked from Kagadi town council and the sub-counties of Nyamarunda, Burora, Bwamiramira, Kyaterekera and Muhorro. The patients, however, on Tuesday protested being poorly fed at the hospital. One of the patients forced his way out of the isolation ward, as the others caused commotion and were calmed by the police, local and district leaders. "It is true that we do not have money to feed these patients, but we are making arrangements to get money and buy them food," one of the health officials said on condition of anonymity. Dr. Kyamanywa said the Medicines Sans Frontiers (Doctors without Borders) had donated plampenats (packed foods) for the patients. But patients had refused to eat the food. The chief administrative officer of Kibaale, Emmanuel Ssenoga said that the district has not received any funds since the financial year started. Meanwhile, hotlines have been created for all people to call, in case they suspect anyone to be infected with the disease.Update; Wednesday, 01 August, 2012 at 18:29 UTC
The number of Ebola cases in Uganda has increased during the past few days, a spokesman from the World Health Organization tells SHOTS. But the outbreak is still limited to a small region. "Accumulatively to date, there are 36 suspected or confirmed cases," WHO's Gregory Hartl says. "All cases are in the Kibaale district," a rural region west of Uganda's capital, Kampala. Laboratory tests, conducted by the Uganda Virus Research Institute and the U.S. Centers for Disease Control and Prevention, have confirmed Ebola infection in 5 people. The specific strain of the virus is Ebola Sudan, which has caused 5 outbreaks in Africa since 1976, including one in Uganda that killed 224 people in 2000. Ebola Sudan typically kills about 50 percent of people infected.
A team, led by the CDC, WHO and Uganda's Ministry of Health, are now at the scene to determine the scope of the outbreak and then control it. This involves a strategy known as contact tracing. "You take every patient who is infected or suspected of infection and ask who they've been in contact with," Hartl explains. "Then you go find those people and do the same." All people in contact with the virus must be isolated and watched for 21 days, CDC spokesman Tom Skinner says. "Only once you've [i.e. all suspects] gone through 2 21-day periods can you be sure that the outbreak is over." This is a massive undertaking, but it's one of the only options for stopping a deadly virus that has no cure or vaccine. The current Ebola outbreak 1st appeared at Ugandan clinics in early July 2012, but it was initially confused with cholera. Doctors didn't suspect Ebola until tests for cholera came back negative and a clinician got sick. "In Ebola outbreaks, health care workers often get infected because you touch somebody and can get the virus," Hartl says. Despite this ease of transmission, he says, Ebola rarely spreads outside a small geographic region. One infected person traveled to a hospital in Kampala, triggering reports that the Ebola outbreak had spread to the capital city. But Hartl says there are no signs that people in Kampala have been infected.Source; http://hisz.rsoe.hu/alertmap/site/?pageid=event_summary&edis_id...
-
Comment by lonne rey on July 30, 2012 at 11:55pm
-
Patients flee hospital over Ebola outbreak
TERRIFIED PATIENTS fled from a hospital in western Uganda as soon as news broke that a mysterious illness that killed at least 14 people in the region was Ebola, one of the world’s most virulent diseases.
http://www.irishtimes.com/newspaper/world/2012/0730/1224321094355.html
-
Comment by Robyn Appleton on July 28, 2012 at 12:24pm
-
EDIS Number: EP-20120727-35948-MYS
Event type: Epidemic
Date/Time: Friday, 27 July, 2012 at 03:17 (03:17 AM) UTC
Continent: Indonesian Archipelago
Country: Malaysia
County / State: State of Sarawak
Area: Bintulu Region
Coordinate: N 3° 11.434, E 113° 5.407
Infected person(s): 177
Minister of Local Government and Community Development Dato Sri Wong Soon Koh yesterday confirmed that there is a cholera outbreak in Bintulu. Speaking to reporters after a briefing by officers from the state Health Department at his office here yesterday, he said the department detected the outbreak on July 14 after a case was confirmed positive with Vibrio Cholerae. “Since July 14, the state Health Department declared there is an outbreak detected in Bintulu. Since then, the state Health Department initiated its investigation to trace all the suspected symptomatic cases. Anyone coming down with diarrhoea and vomiting will be investigated to check whether it is cholera or not,” he added. Based on investigation by the department, the outbreak was believed to have started when three groups of regatta participants from Rumah Gawan, Kampung Jepak and Kampung Hilir in Sebauh, Bintulu used water from Kemena River to wash plates, fish and their hands. “The bacteria from the river had contaminated the food and the hands of the people during the regatta and then continuously spread from person to person and contaminated food and drinks. Now the state Health Department is also suspecting that it is spread from Ramadan Bazaar due to contaminated food and drinks,” he added. He noted that as of yesterday, the department had received 140 cases - 33 positive for cholera, 55 negative and 52 cases still pending result. The youngest patient was one year 11 months old while the oldest was 84 years old. The department also detected nine cases with Vibrio Cholerae but without any symptom. As of yesterday, 177 people had been screened for signs and symptoms of acute gastroenteritis and were given doxycycline, an antibiotic.
On the outbreak, Wong said it was still spreading in Bintulu with 11 localities declared positive for cholera; Rumah Panjang Gawan at Sungai Sebauh, Kampung Jepak, Kampung Sebauh Hilir in Sebauh, Rumah Usah in Sungai Segan, Setinggan Mozako, Kampung Assyikirin, Kampung Sinong in Jalan Masjid, Setinggan Hock Peng Tanjung Kidurong, Batu 10, Jalan Bintulu/Miri, Kampung Baru and Kirana Palm Oil/Brightwood Quarters, Kemena Industrial Estate. “The state Health Department will continue to take all samples from Sungai Kemena and its tributaries as well as food sampling from Ramadan Bazaar and houses. Besides that, the state Health Department will intensify diarrhoea and vomiting surveillance in all health facilities in Bintulu and issue cholera alert to all government, private health facilities in the state whereby when there is increase in number of admission, the state Health Department will investigate whether it is cholera or not,” he said. Wong said attention would also be given to all food handlers in the Ramadan Bazaar in Bintulu to ensure that they meet the department’s health standards, which also requires them to go for cholera screening. “Once they are cleared from the disease, they will be issued health cards and they must bring the health cards with them when they operate the stalls. If they refuse to go for screening, they will be asked to close down their stalls,” he added. For the convenience of the public, a screening centre is opened at the old Bintulu health clinic from 8am to 10pm every day. The department is also using Bintulu Hospital for isolation of severe cases while mild cases and asymptomatic cases would be treated at the national service camp in Samalaju in Bintulu. Wong appealed to the public to give their fullest cooperation to the department to ensure that the outbreak could be contained.Biohazard name: Vibrio Cholera Outbreak
Biohazard level: 2/4 Medium
Source; http://hisz.rsoe.hu/alertmap/site/?pageid=event_summary&edis_id...
-
Comment by Robyn Appleton on July 28, 2012 at 12:22pm
-
EDIS Number:
EH-20120728-35961-ZWE
Event type:
Epidemic Hazard
Date/Time:
Saturday, 28 July, 2012 at 03:34 (03:34 AM) UTC
Continent:
Africa
Country:
Zimbabwe
County / State:
Multiple areas
Area:
Harare (Capital City) and Chitungwiza
Coordinate:
S 18° 0.000, E 31° 3.000
Infected persons:
100
More than 100 people in the Zimbabwean capital Harare and Chitungwiza, a dormitory town 35km southeast of the city, have contracted typhoid this month, and the dilapidated water and sanitation systems are again being blamed for another round of water-borne diseases. According to health officials cited in the local media, 83 cases of typhoid have been confirmed in Chitungwiza and a further 28 in Harare, of which 25 were linked to a supermarket in the Avenues area of the city centre. Portia Manangazira, the chief disease control officer in the Health Ministry, told IRIN that in June 22 cases of suspected cholera, 10 of which were confirmed, were reported in Chiredzi – a town in Masvingo Province close to neighbouring South Africa – and one confirmed case of cholera was reported in Manicaland Province, which borders Mozambique. “We are monitoring the situation very closely to make sure the cholera does not spread. The health sector is on high alert,” she said. A year-long outbreak of cholera in 2008 killed more than 4,000 people and infected about 100,000 others and since then there have been regular outbreaks of waterborne diseases in both urban and rural areas. In January 2012 about 900 Harare residents were diagnosed with typhoid, but no fatalities were recorded.
Biohazard name: Cholera Outbreak
Biohazard level: 2/4 Medium
Source; http://hisz.rsoe.hu/alertmap/site/?pageid=event_summary&edis_id...
SEARCH PS Ning or Zetatalk
This free script provided by
JavaScript Kit
Donate
© 2025 Created by 0nin2migqvl32.
Powered by
![]()
You need to be a member of Earth Changes and the Pole Shift to add comments!
Join Earth Changes and the Pole Shift