Earth Changes and the Pole Shift
Taking Sick
On Jan 15, 1998 ZetaTalk stated that Illness will increase as Planet X approaches. Zetas right again !!!
- ZetaTalk: Take Sick, written Feb 15, 1998.
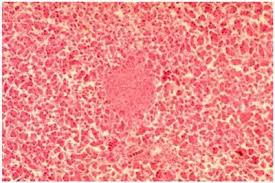
- Increasingly, as the pole shift nears, the populace will take sick. This will take the form of known illnesses occurring more frequently, seemingly depressed immune systems, but will also appear as new and puzzling illnesses not seen before in the memory of man. What is going on here?
The changes at the core of the Earth that have resulted in El Nino weather patterns and white buffalo and deformed frogs also affect man. The germs are on the move. Their carriers are on the move. And thus humans are exposed to diseases that are so rare as to be undocumented in medical journals.
You will see increasing illness, odd illnesses, microbes that travel because an insect is scattering about and spreading germs in places where it normally doesn't travel. 90% of all the illness and distress you're going to see is a natural situation, a natural occurrence. Because of the changing, swirling in the core of the Earth, and this will continue to up-tick until the pole shift.
And reiterated in 1999
- ZetaTalk: Next 3 1/2 Years, written Sep 15, 1999.
- Sickness will slightly increase from where it is today. There is a lot of illness now because people who are already unstable are unable to take the turmoil caused by the increased emanations from the Earth. Some of them have simply sensed what is coming and have decided to die. This is true of animals as well as humans. Sickness will increase, but not to the point where it is going to get exponentially worse.
On Feb 2, 2000 a Washington report confirmed this increase, and published concerns were subsequently reported.
- Diseases From Around World Threatening U.S.
Reuters, Feb 2, 2000 - 30 New Diseases Make Global Debut
At least 30 previously unknown diseases have appeared globally since 1973, including HIV, AIDS, Hepatitis C, Ebola haemorrhagic fever and the encephalitis-related Nipah virus that emerged in Indonesia. Twenty well-known infectious diseases such as tuberculosis, malaria, and cholera have re-emerged or spread since 1973. - Is Global Warming Harmful to Health?
Scientific American, August 2000 - Notably, computer models predict that global warming, and other climate alterations it induces, will expand the incidence and distribution of many serious medical disorders. Disturbingly, these forecasts seem to be coming true.
And since this time, SARS and increased incidence of flesh eating disease,
and entire cruise ships regularly returning to port with the passengers ill with stomach flu have been reported.
Depressed immune systems?
Zetas RIGHT Again!
After the pole shift, there will be many opportunistic diseases that will afflict mankind. This does not require an imagination, as today they afflict mankind after disasters. The primary affliction will be from sewage laden water, which will pollute the drinking water man is forced to use. We have been adamant about mankind distilling their drinking water after the pole shift for this reason. Distillation removes heavy metals as well as killing microbes by the boiling process. Any disease that flourishes in malnourished bodies and in areas of poor hygiene will take advantage of the pole shift disasters. Scurvy due to lack of Vitamin C will occur, with bleeding gums and even death if not corrected. Many weeds are high in Vitamin C and survivors should arm themselves with knowledge about the vitamin content of weeds. Unprotected sex by survivors either taking advantage of the weak, as in rape, or by simple distraction and grief and a lack of contraceptive devices will spread AIDS and hepatitis. Morgellons, which is caused by a synergy of parasites and microbes when the immune system is low will likely increase. There will be outbreaks of diseases which were endemic in the past, such as small pox or measles, but in those survivor communities where the members have been immunized in the past these will be limited and quarantines can help in this regard.
http://www.zetatalk5.com/ning/20no2010.htm
Chile battles youth unrest and typhoid fever outbreak
 September 15, 2011 – SANTIAGO – Chile’s problems dealing with youth unrest over slow education reforms are being compounded by concerns the capital may be in the grip of a typhoid fever outbreak. The government has battled to enforce restraint on law enforcement agencies amid angry student-led protests, which have disrupted urban centers across the country for more than a month. The reforms demanded by youth groups are nowhere near being implemented and protests continue to simmer with support from teachers and workers unions. Now authorities are faced with the more immediate risk of typhoid. Health authorities issued repeated alerts for tougher hygiene checks and controls after they found several people infected and seriously ill with typhoid in the western metropolitan area of Santiago. At least seven cases were confirmed by the Public Health Institute but there were no immediate reports of fatalities. “Typhoid fever is an acute infectious disease triggered by a salmonella bacteria strain,” Institute Director Maria Teresa Valenzuela said. In most cases the infection is caused by consumption of contaminated food and drink or fruit and vegetables grown in areas where contaminated water is used in irrigation. Typhoid fever produces symptoms of high fever, diarrhea or intense headaches. The Santiago region has been prone to typhoid outbreaks since the 1990s when incidence of the disease caused up to 190 cases a year.
September 15, 2011 – SANTIAGO – Chile’s problems dealing with youth unrest over slow education reforms are being compounded by concerns the capital may be in the grip of a typhoid fever outbreak. The government has battled to enforce restraint on law enforcement agencies amid angry student-led protests, which have disrupted urban centers across the country for more than a month. The reforms demanded by youth groups are nowhere near being implemented and protests continue to simmer with support from teachers and workers unions. Now authorities are faced with the more immediate risk of typhoid. Health authorities issued repeated alerts for tougher hygiene checks and controls after they found several people infected and seriously ill with typhoid in the western metropolitan area of Santiago. At least seven cases were confirmed by the Public Health Institute but there were no immediate reports of fatalities. “Typhoid fever is an acute infectious disease triggered by a salmonella bacteria strain,” Institute Director Maria Teresa Valenzuela said. In most cases the infection is caused by consumption of contaminated food and drink or fruit and vegetables grown in areas where contaminated water is used in irrigation. Typhoid fever produces symptoms of high fever, diarrhea or intense headaches. The Santiago region has been prone to typhoid outbreaks since the 1990s when incidence of the disease caused up to 190 cases a year.
Epidemic Hazard in India on Saturday, 17 September, 2011 at 03:16 (03:16 AM) UTC.
| Description | |
| The Department of Health and Family Welfare has informed that it had received a message through telephone on 12th September 2011 of an outbreak of fever of unknown cause leading to three deaths at Poilwa village, Peren District. Immediately the State Rapid Response Team (RRT) of Integrated Disease Surveillance Project (IDSP), Nagaland, comprising of Dr. John Kemp (State Surveillance Officer), Dr. Sao Tunyi (Epidemiologist), Dr. Kevisevolie Sekhose (Epidemiologist), and Venezo Vasa (Entomologist) conducted an outbreak investigation at Poilwa village. The team collected three samples from suspected cases out of which all the three were tested positive for Scrub Typhus. Till date, there are 9 cases with 3 deaths. This was stated in a official press note issued by Dr. Imtimeren Jamir, the Principal Director, Directorate of Health & Family Welfare, Kohima. Scrub Typhus is Rickettsial disease caused Orientia tsutsugamushi and transmitted by the bite of mite called Leptotrombidium deliense. In Nagaland, it was formerly detected by IDSP with Central Surveillance Team at Longsa village Mokokchung in 2006, and in Porba village of Phek District in 2007. The State RRT team carried out the outbreak investigation along with doing and entomological survey. The patients were treated with appropriate medicines and awareness and preventive measures were communicated with the villagers. The concerned local health authorities and programs are informed for further necessary action. The mop-up operation is being carried out by the National Vector Borne Disease Control Program. | |
| Biohazard name: | Typhus (Scrub) |
| Biohazard level: | 3/4 Hight |
| Biohazard desc.: | Bacteria and viruses that can cause severe to fatal disease in humans, but for which vaccines or other treatments exist, such as anthrax, West Nile virus, Venezuelan equine encephalitis, SARS virus, variola virus (smallpox), tuberculosis, typhus, Rift Valley fever, Rocky Mountain spotted fever, yellow fever, and malaria. Among parasites Plasmodium falciparum, which causes Malaria, and Trypanosoma cruzi, which causes trypanosomiasis, also come under this level. |
| Symptoms: | - After bite by infected mite larvae called chiggers, papule develops at the biting site which ulcerates and eventually heals with the development of a black eschar. - Patients develop sudden fever with headache, weakness, myalgia, generalized enlargement of lymph nodes, photophobia, and dry cough. - A week later, rash appears on the trunk, then on the extremities, and turns pale within a few days. - Symptoms generally disappear after two weeks even without treatment. - However, in severe cases with Pneumonia and Myocarditis, mortality may reach 30% Diagnosis - The most commonly used test for diagnosis is Wel-Felix Test, which is available at State IDSP laboratory, Kohima. - More specific serological tests like detection of IgM can also be done for diagnosis. |
| Status: | confirmed
|
Turns out, the plague isn't just ancient history. New Mexico health officials recently confirmed the first human case of bubonic plague — previously known as the "Black Death" — to surface in the U.S. in 2011.
An unidentified 58-year-old man was hospitalized for a week after suffering from a high fever, pain in his abdomen and groin, and swollen lymph nodes, reports the New York Daily News. (Officials declined to say when the man was released from the hospital.) A blood sample from the man tested positive for the disease.
http://healthland.time.com/2011/05/10/first-case-of-bubonic-plague-in-2011-appears-in-new-mexico/
Epidemic Hazard in USA on Saturday, 17 September, 2011 at 03:33 (03:33 AM) UTC.
| Description | |
| Umatilla County health officials today confirmed a case of plague in an adult male county resident. He may have been infected while hunting in Lake County, noted Sharon Waldern, clinic supervisor for the county’s public health department. “Lake County had two cases of human plague last year.” The man has been hospitalized and is receiving treatment, Waldern noted. “People need to realize he was never considered contagious and he started treatment fairly quickly.” Plague is spread to humans through a bite from an infected flea. The disease is serious but treatable with antibiotics if caught early, officials said. Plague can be passed from fleas feeding on infected rodents and then transmitted to humans. Direct contact with infected tissues or fluids from handling sick or dead animals can pass the disease, as well as through respiratory droplets from cats and humans with pneumonic plague, officials said in a press release. Some types are spread from person to person, but that is not the case here, Waldern said. Symptoms typically develop within one to four days and up to seven days after exposure and include fever, chills, headache, weakness and a bloody or watery cough due to pneumonia, enlarged, tender lymph nodes, abdominal pain and bleeding into the skin or other organs. Plague is rare in Oregon. Only three human cases have been diagnosed since 1995 and they all recovered. Last year two human cases of plague were diagnosed in Lake County. As far as she knows, this is the first ever incident in Umatilla County. “In this recent case it is important to stay away from flea-infested areas and to recognize the symptoms. People can protect themselves, their family members and their pets,” said Genni Lehnert-Beers, administrator for Umatilla County Health Department. “Using flea treatment on your pets is very important, because your pets can bring fleas into your home.” People should contact their health care provider or veterinarian if plague is suspected. Early treatment for people and pets with appropriate antibiotics is essential to curing plague infections. Untreated plague can be fatal for animals and people. Antibiotics to prevent or treat plague should be used only under the direction of a health care provider. Additional steps to prevent flea bites include wearing insect repellent, tucking pant cuffs into socks when in areas heavily occupied by rodents, and avoiding contact with wildlife including rodents. |
|
| Biohazard name: | Plague (Bubonic) |
| Biohazard level: | 4/4 Hazardous |
| Biohazard desc.: | Viruses and bacteria that cause severe to fatal disease in humans, and for which vaccines or other treatments are not available, such as Bolivian and Argentine hemorrhagic fevers, H5N1(bird flu), Dengue hemorrhagic fever, Marburg virus, Ebola virus, hantaviruses, Lassa fever, Crimean-Congo hemorrhagic fever, and other hemorrhagic or unidentified diseases. When dealing with biological hazards at this level the use of a Hazmat suit and a self-contained oxygen supply is mandatory. The entrance and exit of a Level Four biolab will contain multiple showers, a vacuum room, an ultraviolet light room, autonomous detection system, and other safety precautions designed to destroy all traces of the biohazard. Multiple airlocks are employed and are electronically secured to prevent both doors opening at the same time. All air and water service going to and coming from a Biosafety Level 4 (P4) lab will undergo similar decontamination procedures to eliminate the possibility of an accidental release. |
| Symptoms: | |
StatuThe Black Death: Bubonic Plague
|
confirmed http://hisz.rsoe.hu/alertmap/site/?pageid=event_desc&edis_id=EH-20110917-32359-USA
|
Starr DiGiacomo
Dreaded Diarrhea Diseases for Toddlers: Rotavirus and Other Agents 2011
Apr 19, 2011
According to the Centers for Disease Control CDC there has been a dramatic uptick in voluntarily reported incidences of rotavirus in the Midwestern and Western Regions during late spring, 2011. Rotavirus and other viral gastroenteritis agents and protozoan parasites are responsible for diarrhea, vomiting and dehydration in infants, children and the elderly, according to Brown University. Rotavirus is highly contagious and transmitted through the fecal-oral route. Anti-bacterial soap hand washing is not sufficient to eliminate the disease. Instead, epidemiologists recommend alcohol based products for cleaning affected areas. Each year in the United States, more than 3 million children are diagnosed with rotavirus and over 55,000 require hospitalization for the disease. World-wide rotavirus is the leading cause of children's death in third world nations.
Diagnosis:
Rotavirus can be tricky to diagnose in the most vulnerable age groups ages six months to two years and the elderly because the symptoms mimic numerous other agents and parasites, according to the National Foundation for Disease Control, the following symptoms requires further testing and treatment to prevent dehydration by a competent medical doctor. A physician should be contacted immediately if any signs of dehydration are present or if the symptoms last more than 48-hours. There is no antibiotic treatment available for rotavirus.
http://www.associatedcontent.com/article/7982085/dreaded_diarrhea_d...
Sep 19, 2011
Starr DiGiacomo
Climate Change and Infectious Disease: Is the Future Here?
atherine M. Cooney
Catherine M. Cooney, a science writer based in Washington, DC, has written for Environmental Science & Technology and Chemical Watch.
Environ Health Perspect 119:a394-a397 (2011). http://dx.doi.org/10.1289/ehp.119-a394 [online 01 September 2011]
After kayaking on Vancouver Island’s eastern shore, a 45-year-old woman’s headaches and night sweats were little indication that she had been exposed to a rare and dangerous fungus while on the water. Her doctors, mystified as to the cause of the symptoms, didn’t recognize that the infection was Cryptococcus gattii—a species of pathogenic yeast—until shortly before her death in 2002.1
Most cases of C. gattii have been reported in the warmer climates of Australia, Asia, Africa, and Southern California. But at least two strains of the fungus are now affecting humans, pets, and wild animals in the U.S. Pacific Northwest.2 From January 2004 through July 2010, a total of 15 people died from C. gattii infection, according to the Centers for Disease Control and Prevention (CDC), and 60 human cases of the illness were reported in Oregon, Washington, California, and Idaho.3 Despite the alarming sound of the disease, public health officials in Oregon have urged residents not to consider the spread of C. gattii as a health emergency—although the fungus is present in the wild, few people have become seriously ill with this infection, and even fewer have died, says Oregon state epidemiologist Katrina Hedberg.
Nevertheless, the mere presence of this foreign species so far from its home raises questions. Reports suggest the fungus may have been exported from its native habitat on commercially valuable trees such as eucalyptus and ornamental Ficus species.4 “We don’t know exactly why the [Pacific Northwest] outbreak emerged,” says Edmond Byrnes, a postdoctoral fellow at the Johns Hopkins University School of Medicine who has studied the fungus.5 “One of the more current hypotheses is that climate change is one of the factors that should be considered.” Byrnes explains that C. gattii may be able to establish itself in the Pacific Northwest region because of milder winters with daily average temperatures above freezing.
C. gattii is one of several pathogens whose spread is hypothesized to be linked to climate change. Like many aspects of climate change, the connection with infectious disease involves controversy. Some scientists argue that improved climate models may give a false impression that climate change is driving a spread in infectious diseases; others point to human activity and other factors as far more important determinants than climate.6,7,8,9
But health practitioners know that a myriad of factors affect the spread of any disease, and many of these—including human migration, poverty, water and air quality, land use decisions, ecological change, the strength of the local public health system, and even access to air conditioning—are themselves intertwined with climate change.10 Moreover, says Jonathan Patz, a professor of environmental studies and population health sciences at the University of Wisconsin–Madison, “So many infectious diseases are sensitive to climate that if the majority of the climatologists around the world are telling us that climate is changing and will continue to change under the scenario of global warming, then disease incidence will change.” Several scientific studies and reports suggest these proposed future effects of climate change are in fact already occurring.11
Diseases of Interest
Considering climate change and extreme weather events when analyzing the spread of disease is a fairly new idea. In one of the first papers to call attention to the potential connection, published in 1989, author Alexander Leaf listed immune system depression, health care and sanitation deficiencies, pollution, population shifts, malnutrition, vector shifts, and contaminated water supplies as factors that could spur a rise in infectious diseases in a warming climate.12 Studies published as part of a series in The Lancet in the fall of 1993 first began to link increased cases of infectious disease to longer seasons, hotter temperatures, and increased rainfall.13,14,15 Studies published since then have coupled aspects of climate change to increased outbreaks of viral illnesses such as West Nile virus (WNV) and dengue fever, and to outbreaks of bacterial illnesses such as cholera and salmonellosis.10 In 1996 the Intergovernmental Panel on Climate Change (IPCC) for the first time included a chapter on public health effects in its report.16
To make a firmer determination about links between climate change and infectious disease, researchers need high-quality data collected over long periods detailing changes in the numerous factors that go into the spread of disease. But those data haven’t been collected. “That is one reason some of us look at cases where [there are] unseasonable conditions, like in an El Niño where there are unseasonal rain or drought conditions or unusually high temperatures,” Patz says. “We look at that and say, as scientists, okay what did that extreme weather pattern do to disease? If we can study what happens to disease in extreme weather events, it gives us a window into the future [where such extremes are expected to become more common].”
Most public health officials contacted for this article agree that climate change and extreme weather events will move more infectious diseases northward. Warmer winters and high-latitude warming—occurring twice as fast as overall warming17—are already contributing to shifts and expansions of vector ranges.18 In addition, extreme weather events—occurring with greater frequency and intensity19—are often associated with outbreaks of water-, mosquito-, and rodentborne diseases,20 says Paul Epstein, associate director of Harvard’s Center for Health and the Global Environment.
But predicting how the interaction of factors will play out is not always straightforward. According to the World Health Organization (WHO) Scientific Working Group, dengue is the most rapidly spreading vectorborne disease in the world, with the average annual number of reported cases increasing by more than 7.5 times between 1970–1979 and 2000–2005.21 Malaria, on the other hand, is decreasing in all regions in response to highly targeted control efforts—in 2009 there were an estimated 225 million cases and 781,000 deaths worldwide, down from 233 million cases and 985,000 deaths in 2000.22 In the World Malaria Report 2010 the WHO stated, “A realistic view of what would have happened without control activities . . . cannot be established from the data currently available,” but suggested that, absent control activities, short-term climate variations could be expected to affect disease trends.22
Lyme disease, spread by ticks carrying the bacterium Borrelia burgdorferi, has been expanding for decades in the United States, but it is difficult to know how much of that expansion is a result of infected ticks expanding their geographic range versus growing awareness and better detection of the disease. It is clearly both, says Richard S. Ostfeld, a disease ecologist with the Carey Institute of Ecosystem Studies in Millbrook, New York. “We know [Lyme disease] has spread into the mid-Atlantic states, into Maryland and Virginia and north into New Jersey and New York and southern Canada,” he says. “It is possible that the spread northward is influenced by a warming climate, but that wouldn’t explain the spread southward. We just don’t know what the other factors are.”
Other diseases are predicted to become more prevalent as a result of climate-related changes in water and food sources. Water contamination from flooding can cause shortages of clean water that lead to the spread of diarrheal diseases such as cholera as well as enteric diseases such as typhoid.23 Not having enough water for cleaning and bathing can cause infections such as scabies24 and trachoma,25 whereas drinking too little water can lead to harmful infections of the bladder and kidneys.26 Warm temperatures and rainfall have also been tied to the spread of foodborne contaminants. For example, contamination of crops with aflatoxins—potent mycotoxins produced by Aspergillus flavus fungi that can cause developmental and immune system suppression, cancer, and death—is linked both to increased rainfall and to drought.27
One thing that seems fairly clear is that not all areas will see uniform shifts in infectious diseases; these, like other climate-related changes, will be highly dependent on local factors.10 “In some areas [in the United States] we expect to see a disease increase, and in others areas we expect to see a decrease. How climate change will affect that is really a wildcard at this time,” says Ben Beard, associate director for climate change at the CDC’s National Center for Emerging and Zoonotic Infectious Diseases.
Source:
http://ehp.niehs.nih.gov/119-a394/
Sep 19, 2011
Starr DiGiacomo
Measles Outbreak: Cases Rise in Europe and U.S.
http://healthland.time.com/2011/05/17/measles-outbreak-cases-rise-i...
Sep 19, 2011
Starr DiGiacomo
The U.S. saw an uptick in food poisoning cases last year, and the main culprit was salmonella.
The latest figures from the national Centers for Disease Control an... show that more than 19,000 people in 10 states -- including Oregon -- fell ill after eating contaminated food last year, compared with 17,500 the year before. Salmonella accounted for more than 8,000 of those illnesses and nearly 30 deaths.
"Salmonella is the single most important foodborne disease right now," said Dr. Thomas Frieden, a CDC director. "Prevention will require action from the farm to the table."
Salmonella infections have not decreased over the past 15 years; in fact, they've risen since 2009. There are more than 2,500 strains of the bacteria, which is found in a wide range of food, from poultry and eggs to pork, beef, vegetables and nuts.
"Salmonella is a big challenge because it's spread through so many foods," said Michael Taylor, deputy commissioner for foods at the Food and Drug Administration.
Taylor said rules being enacted through the Food Safety Modernization Act, which went into effect in January, should help reduce illness.
The 10 states that report to the CDC -- California, Colorado, Connecticut, Georgia, Maryland, Minnesota, New Mexico, New York, Oregon, and Tennessee -- marked a drop in infections of E. coli O157:H7 last year. But there could be a rise in infections caused by other toxic strains that many labs do not tract because of the cost of adding the testing kit.
The outbreak in Germany, which so far has sickened more than 2,400 and killed 24, was traced to a mutant E. coli strain that has rarely been seen worldwide and has never been reported in the United States.
The CDC does not expect the outbreak to jump to the United States but highly toxic E. coli strains could end up here, epidemiologists say.
http://www.oregonlive.com/health/index.ssf/2011/06/oregon_9_other_s...
Sep 19, 2011
Starr DiGiacomo
Latest health alerts for international travelers
Sep 19, 2011
Starr DiGiacomo
Link to that article
http://www.passporthealthusa.com/localvaccines/travel-health-alerts...
Sep 19, 2011
Starr DiGiacomo
The CDC on Emerging Infectious Diseases
Disease Emergence the World Over
http://wwwnc.cdc.gov/eid/pdfs/vol17no9_pdf-version.pdf
Sep 19, 2011
Starr DiGiacomo
http://www.tehrantimes.com/index.php/component/content/article/2711
Sep 19, 2011
Starr DiGiacomo
Meningococcal Disease Outbreak in Northland
It has been revealed that Northlanders shall now be given free vaccination against the infection of meningococcal C disease. This has come as a preventive measure by the health facility of the area after recent cases of this disease were discovered since July and there have even been two deaths due to the same in recent times.
It has now been announced as an outbreak and the Northland District Health Board campaign has been launched to fight the disease. Under this there are free vaccinations being given to the people of the vicinity and this shall commence from vaccination to high-school students in the areas, because they happen to be the ones at an increased risk of the virus.
This is going to be a different strain of vaccination from what had been given to patients during the outbreak of meningococcal disease of type b in the year 1991-2008 in New Zealand.
"Following expert advice, and in consultation with the Ministry of Health, we have decided to launch a vaccination campaign to help control this outbreak and prevent more cases of disease”, revealed Dr. Clair Mills the medical officer of health in the area.
http://frenchtribune.com/teneur/117206-meningococcal-disease-outbre...
Sep 19, 2011
Starr DiGiacomo
Dengue outbreak hits Bahamas, CDC says
http://www.washingtonpost.com/national/health-science/dengue-outbre...
Sep 19, 2011
Starr DiGiacomo
Cholera outbreak in rain-hit areas: three die, 24 confirmed cases
http://www.pakistantoday.com.pk/2011/09/cholera-outbreak-in-rain-hi...
Sep 19, 2011
Starr DiGiacomo
500 contacted by health workers about possible measles exposure
End of week marks incubation period
The next one to two weeks could determine whether Milwaukee sees a measles outbreak, or whether the measles is limited to the two cases already confirmed, a city health official said Friday.
No new measles cases have been confirmed in recent days, but the end of this week marks the typical incubation period for anyone exposed to a Milwaukee child with measles to begin developing symptoms, said Paul Biedrzycki, the city's director of disease control and environment health.
"After next Friday, we may be out of the woods," Biedrzycki said. "We're grateful we're not seeing more cases, but we're very cautious about saying we could be out of the woods."
Surveillance will continue until late October. More than 500 people have been notified - some in door-to-door efforts by public health workers - because they may have been exposed to measles at one of eight locations the child visited while contagious.
Nearly 200 of those people were in the same south side building from 9 a.m. to 1 p.m. on Sept. 2. A Milwaukee adult is confirmed to have picked up measles from the child at this location.
"You don't have to have long, or close, contact to be exposed," Biedrzycki said. Being in a building with offices that share the same air ventilation system is enough exposure because measles is highly contagious, he said.
Refugee camp outbreak
The child's family moved to the city at the end of August. It's believed that the child contracted the disease at a refugee camp where there was a measles outbreak.
Since 2000, one in every 250 Americans who got measles died. An outbreak in Wisconsin in 1989-'90 killed six children - four babies, a 10-year-old and an 11-year-old. The last outbreak in Milwaukee in 2008 involved eight cases and no fatalities.
The first symptom of measles usually is fever. The measles rash typically doesn't appear until about 14 days after exposure and two to three days after the fever begins.
Vaccination is considered 99% effective against measles, and city officials are encouraging anyone whose vaccinations are not up-to-date to get immunized.
Officials earlier this week were investigating three or four suspected cases, but those cases were cleared. A handful of new suspected cases is now being investigated, Biedrzycki said Friday. Possible exposure occurred in multiple locations the child with measles visited.
None of the possible new cases involves hospitalizations. The child with measles was released from a hospital last week.
The Milwaukee adult was in a Social Security Administration office in a south side building where the child visited, according to Biedrzycki. The building at 1710 S. 7th St., houses both a Social Security Administration office and a Planned Parenthood office.
While the child was not in the Planned Parenthood office, anyone in that office could have been exposed because it shares the same air ventilation system as the Social Security office, Biedrzycki said.
City's vulnerability
City officials are concerned about Milwaukee's vulnerability to vaccine-preventable diseases such as measles because of its low immunization rate for young children.
The city's vaccination rate for school-age children is 79% to 80%. For children ages 1 to 3 years, the rate is even lower - about 50%.
Several clinics are offering free vaccinations, including two clinics open Saturday.
Since the first measles case was confirmed last week, turnout at the vaccination clinics has been low, Biedrzycki said.
Adults born during or after 1957 who do not know their measles vaccination status should consider vaccination, the health department advises.
People with fever and
Sep 19, 2011
Starr DiGiacomo
Since 16 August 2011, eleven cases of travel associated Legionnaires’ disease have been notified to the European Legionnaires’ disease surveillance network (ELDSNet). All cases stayed at four different accommodation sites in the touristic town of Lazise, Italy, between 7 July 2011 and 31 August (last departure). The countries reporting cases are the Netherlands (5 cases), Austria (1 case), Italy (4 cases) and Denmark (1 case). The average age of the cases is 54 years (min 42-max 78) and the gender distribution is 10 males / 1 female. Precautionary control measures such as hyperchlorination and switching off of all aerosol producing devices (spa pools, decorative fountains, sprinklers) have been taken.
ECDC is monitoring this situation closely. More information will be posted on the website shortly.
http://ecdc.europa.eu/en/activities/sciadvice/Lists/ECDC%20Reviews/...
Sep 19, 2011
Starr DiGiacomo
Experts to study disease outbreak
MALAPPURAM: Expert team from Kozhikode Medical College will visit Vandur region on Thursday to study the rare parasitic disease Schistosomiasis. The outbreak of the disease has been reported for the first time in the district. Following the, reported first time in the district., , to study the rare disease in detail, on Thursday.
The team which will comprise doctors from departments of microbiology, pediatrics, and community medicine, will examine the samples collected from a boy, who has been admitted to a private hospital in Manjeri with the symptoms of the disease. The parasitic disease caused by Trematode Flatworms of the genus 'Schistosoma', is a very rare disease in the country. It is commonly seen in sub-Sahara areas of Africa and the Gulf countries.
According to Dr. Abdul Jaleel, pediatrician of Malabar Hospital in Manjeri, the boy was admitted to the hospital with all the symptoms of the disease. It was the medical experts in the district who conducted a detailed examination of the samples and confirmed the disease. The district medical officer Dr. A. Sameera and experts from MES Medical College, Perinthalmanna, also examined the patient at the hospital.
http://articles.timesofindia.indiatimes.com/2011-09-14/kozhikode/30...
Sep 19, 2011
Starr DiGiacomo
With confirmation of another two polio cases from Balochistan here on Monday, the explosive outbreak of the crippling disease is continuing in the Quetta block, which constitutes a major threat to other areas within the province as well as the country at large.
The Prime Minister s Monitoring and Coordination Cell for Polio Control has advised the health secretary of Balochistan to immediately conduct mop-up activities in and around areas where the new cases have been reported so that other children in the vicinity are protected and further spread of the infection can be brought under control.
The latest cases, which are from Pishin and Loralai districts, have taken the total number of polio cases countrywide in 2011 so far to 89 (88 type-1 cases and 1 type-3 case). Loralai is a newly-infected district.
According to details, Yasin, an 18-month-old male child residing in Union Council (UC) Karbala of tehsil Pishin, had onset of paralysis on August 29, 2011. As per recall of the parents, the child has not received any dose of oral polio vaccine (OPV) due to refusal on part of the parents.
This is the ninth polio case from district Pishin this year and the third from UC Karbala. In fact, all the 12 polio cases in district Pishin during the last three years were reported from tehsil Pishin. It is reported that the three cases in UC Karbala belong to an area which has a significant number of families refusing to polio vaccination during the Supplementary Immunisation Activities (SIAs).
Moreover, the quality of vaccination campaigns in district Pishin has been a major concern. Pishin could not achieve 95% finger marking coverage in 5 of the 7 SIAs conducted in 2011. UC Karbala could not achieve 95% finger marking coverage in 2 campaigns. According to experts, high proportion of UCs below 90% finger marking coverage during most of the campaigns indicates performance gaps at the sub-district level.
Acute Flaccid Paralysis (AFP) surveillance data for 2011 shows that none of the 13 non-polio AFP cases aged 6-23 months received three routine OPV doses (based on parents recall), indicating gaps in the routine immunisation.
The latest case from Loralai is Shahzad Khan, a 12-month-old male child who had onset of paralysis on September 5, 2011. The child resides in Killi Ghasiabad, UC Dukki Saddar, in tehsil Dukki. As per recall of the parents, the child had not received any OPV dose due to parental refusal. This is the first polio case reported from district Loralai after about three years; the last reported polio case had onset of paralysis in July 2008. continued....
http://www.thenews.com.pk/TodaysPrintDetail.aspx?ID=68605&Cat=6
Sep 20, 2011
Starr DiGiacomo
Polio Outbreak and more
As Miguel has pointed out, Polio has now spread to China.
September 21, 2011
Big news today is that China has experienced a polio outbreak. The disease apparently made its way to China via Pakistan. This is the first polio outbreak in China since 1999. A disease that was once thought completely eradicated has now reared its ugly head.
http://healthcare-economist.com/2011/09/21/polio-outbreak-and-more/
Sep 21, 2011
Starr DiGiacomo
Fear of Plague Prompted Pesticide Use at Malibu High, Principal Says
The pesticides were distributed in pellet-form to minimize the risk to humans, school district and health officials say.
School district officials said the recent use of pesticides at Malibu High School that triggered heated community discussion was done to comply with the county's demand that the school's ground squirrel population be controlled. The pesticides were distributed in pellet-form into the animals' burrows, minimizing the human health risks, school district and state health officials said.
An annual county inspection of Malibu High on Aug. 19 "revealed an infestation of ground squirrels," said Jan Maez, the Santa Monica-Malibu Unified School District's chief financial officer.
Following the inspection, the county issued the SMMUSD an enforcement notice that the ground...cont. story
http://malibu.patch.com/articles/fear-of-plague-prompted-pesticide-...
I can't remember a time here in the US we had to discuss precautionary plague measures. Malibu HS is taking this scare very seriously. The CDC must know a bit more than they are sharing right now.
Sep 22, 2011
Starr DiGiacomo
Meningococcal disease claims another victim
Published: 9:23AM Thursday September 22, 2011
A young man has died of meningococcal septicaemia - Wellington's fifth case of meningococcal disease in the past few months, and the 10th this year.
Wellington Public Health said all of the cases of the illness have been in people under 20.
It is attributing the blip to the season and also a sharp rise in respiratory illnesses.
Another contributing factor could be that the flu and onset of meningococcal disease present similar symptoms similar so people can be slow to identify the seriousness of the illness, it said.
The young man's death follows a 19-year-old Wellington student who died from meningococcal disease earlier this year. Public health has not released the age of the latest victim.
Penelope Lake, a student at Victoria University, died in Wellington Hospital in April after coming down with flu-like symptoms the day before.
Northland has also had an outbreak of the disease - an 18-year-old Whangarei teenager died in Whangarei District Hospital's intensive care unit and a 14-month-old Ruakaka boy died in Starship Hospital in Auckland last month.
Northland cases prompt vaccination programme
In a bid to control the sharp jump of cases in Northland, health authorities announced earlier this month they were running a one-off meningococcal vaccination programme throughout the region.
The vaccination programme aims to vaccinate at least 85% of everyone in Northland aged 12 months to 20 years.
The programme will start on September 26 and is expected to run for about 10 weeks.
In another case a young child died in Rotorua Hospital from meningococcal disease last month, and the chief executive of Fulton Hogan, 48-year-old Bill Perry, died in Christchurch after contracting meningococcal C.
Children, teenagers and young adults are most at risk of meningococcal disease.
Meningococcal disease symptoms include fever, headache, aversion to light, vomiting, a rash that does not fade when pressed, confusion and a decreased level of consciousness.
Click here for more information about meningococcal disease.
http://tvnz.co.nz/national-news/meningococcal-disease-claims-anothe...
Sep 22, 2011
Starr DiGiacomo
CDC says 8 people are dead in listeria outbreak traced to Colorado cantaloupes
By Associated Press, Published: September 21
WASHINGTON — The death toll has risen to eight in an outbreak of listeria traced to Colorado-grown cantaloupes, officials said Wednesday.
The Centers for Disease Control and Prevention said that a person in Maryland died from eating the tainted produce. Four deaths have been reported in New Mexico and two in Colorado, and one person has died in Oklahoma.
The CDC said 55 people in 14 states have now been confirmed as sickened from eating the cantaloupes. On Monday, the CDC reported four deaths and 35 illnesses in 10 states.
continued story....
http://www.washingtonpost.com/business/cdc-says-8-people-are-dead-i...
Sep 22, 2011
Starr DiGiacomo
California measles cases hit a 10-year high
http://latimesblogs.latimes.com/lanow/2011/09/measles-california-de...
Sep 22, 2011
Starr DiGiacomo
More at-risk flights identified in measles outbreak
Published: 10:45AM Thursday September 22, 2011 Source:
Passengers are being urged to check their immune status as more flights with measles-infected passengers have been revealed.
Health authorities have announced three more flights carried an infected passenger.
The latest flights are:
- Air New Zealand NZ419 from Auckland to Wellington on Friday, September 9 at 12:30pm
- Air New Zealand NZ428 frin Wellington to Auckland on Saturday, September 17 at 2:30pm
In addition to these flights announced earlier today:
- Jetstar JQ263 from Auckland to Wellington on Monday, September 12 at 6:40am
- Air New Zealand NZ464 from Wellington to Auckland on Monday, September 12 at 5.30pm
- Jetstar JQ244 from Christchurch to Auckland on Sunday, September 18 at 7.10am
This is following an earlier warning this week from the Auckland Regional Public Health Service that a passenger on a Jetstar flight JQ265 from Auckland to Wellington and an Air New Zealand flight NZ446 from Wellington to Auckland was in the early, infectious stages of the disease.
Medical Officer of Health, Dr Richard Hoskins said "anyone who travelled on those flights should check their immune status and if in doubt call their GP."
"Immunisation is the most important way to prevent measles. People who haven't been immunised are at risk of catching the disease."
Seven more Aucklanders have been diagnosed with the highly infectious disease, which is spread by sneezing or coughing, since yesterday.
There have been 164 cases since the outbreak began four months ago and 24 of those have required hospitalisation.
Thirty six people are in quarantine after contact with someone with measles.
Another case of measles in a baby boy was identified in Christchurch.
Canterbury Medical officer of Health Dr Ramon Pink said they are investigating the case and it is unrelated to a case confirmed over the weekend.
Pink said the infant lives in a semi-rural environment and has no connection with the other patient who is a university student.
Health authorities are connecting the rise in cases to extra Rugby World Cup 2011 travel.
http://tvnz.co.nz/national-news/measles-risk-identified-in-more-fli...
Sep 22, 2011
Starr DiGiacomo
Warnings on speed of deadly disease
Waikato mother Vicki Ellis died within 25 hours of the first symptoms of meningicoccal disease. Photo / Supplied
This disease took Vicki Christina Ellis so quickly her two teenage sons had no chance to say goodbye to her.
The 34-year-old died in Waikato Hospital of group C meningococcal disease, 25 hours after experiencing the first symptoms.
She is one of nine people to have become sick with meningococcal disease in the Waikato this year, and one of two deaths.
A young child died in the hospital on August 13. Ms Ellis died on June 9.
Her mother, Dawn Ellis, of Thames, spoke publicly about her daughter's death yesterday, because of an outbreak of the group C disease in Northland which has led the area's health board to undertake mass vaccination of children and teenagers.
Wellingtonians were yesterday warned by their public health service to be alert for symptoms of the disease, after the death of one person and the infection of four others in the area this month.
But Northland, where the incidence is at least three times what is considered usual, is the only area experiencing higher numbers of cases than usual.
Ms Ellis worked at Noel Leeming at the Base. She lived in Hamilton with her sons, Clayton, now aged 17, and Nicholas, 13, her partner Jon Mansfield, and her sister Debbie.
Mrs Ellis said her daughter's death had been a terrible shock.
"She's got the two boys and of course they didn't get to say goodbye to her because they didn't know she was that sick. Nobody realised, even her partner."
Ms Ellis started feeling unwell and vomited the day before she died.
"[Debbie] had to call the ambulance because she [Vicki] was having a fit. She said she was hot and cold.
"Then Debbie couldn't understand her. She was waving her arms around as if she was hurting somewhere but Debbie couldn't get out of her what was the matter.
"By the time they got her into hospital, I don't think she came round after that."
Mrs Ellis arrived at the hospital at 4 o'clock the following morning.
"We had to wait around because they were doing tests - they thought she might have blood poisoning.
"When we went in it just looked like she was sleeping. She didn't have any rashes or anything like they thought she might have.
"We didn't get to speak; even [Debbie] didn't get to talk to her after that. [Debbie] thought she was in an induced coma, but I think it was the bug had taken over. They had her on IVs [intravenous drips] and oxygen, the whole thing."
Mrs Ellis said the infection took hold quickly. . "My husband thought it was about 25 hours and that was it."
Symptoms of meningococcal disease, a bacterial infection, can include high fever, sleepiness, muscle and joint pain, bad headache, stiff neck, aversion to bright lights, and an infant refusing feeds. A rash is a common late symptom. The disease can be readily treated by antibiotics if detected early.
KILLER BUG
* Wellington-Wairarapa region: 10 cases; 1 death.
* Auck
Sep 22, 2011
Starr DiGiacomo
KILLER BUG continued
* Wellington-Wairarapa region: 10 cases; 1 death.
* Auckland region: 28 cases; 1 death.
* Waikato: 9 cases; 2 deaths.
* Northland: 6 cases since July; 2 deaths.
http://www.nzherald.co.nz/health/news/article.cfm?c_id=204&obje...
Sep 22, 2011
Starr DiGiacomo
The story from the link below which I had a hard time pasting here.
(AP) HANOI, Vietnam — More than a dozen kindergartens in Vietnam have closed to deal with an outbreak of hand, foot and mouth disease that has killed 109 children and sickening more than 52,000 this year, an official and state-run media said Monday.
Ten kindergartens in Hau Giang province were shut for 10 days to clean and check the students' health, said Nguyen Van Muoi, head of the provincial preventive medicine center. Four schools reopened last week, he added.
The southern province has had 361 cases since June, and some 50 children are hospitalized. He blamed the increase on the virus' spread after children returned to school from summer break.
"I hope with this measure (closing the preschools), the new cases will drop," Muoi said.
At least three more kindergartens in the southern Bac Lieu province and the central highland province of Dak Nong also have been closed, Monday's Vietnam News reported.
The Health Ministry says more than 2,000 new cases of hand, foot and mouth disease are being reported each week. In a typical year, the virus infects up to 15,000 children in Vietnam and kills 20 to 30 of them.
The Health Ministry has recorded 52,321 cases and 109 deaths in the country as of Sept. 15. A more severe strain called enterovirus 71, or EV-71, was identified earlier in about a third of sampled cases. It can result in paralysis, brain swelling and death.
The World Health Organization has said three-quarters of the deaths have been children younger than 3 years old.
The virus is named from its telltale symptoms, including rash, mouth sores and blisters on the hands and feet. It is spread by sneezing, coughing and contact with fluid from blisters or infected feces.
No vaccine exists, but the illness is typically mild and most children recover quickly. The disease is caused by enteroviruses in the same family as polio.
Sep 26, 2011
Starr DiGiacomo
Unusual food born diseases on the uptick
Cargill Ground Turkey Positive for Outbreak Strain
A sample of ground turkey from Cargill's Sept. 11 recall of 185,000 pounds of ground turkey tested positive for the Salmonella Heidelberg outbreak strain (XbaI PFGE pattern 58/BlnI pattern 76), the U.S. Department of Agriculture's Food Safety and Inspection Service (FSIS) announced late Tuesday.
The ground turkey is implicated in an outbreak that as of Sept. 14 had infected 119 people in 32 states with Salmonella Heidelberg, according to the Centers for Disease Control and Prevention.
http://www.foodsafetynews.com/2011/09/cargill-ground-turkey-positiv...
Sep 28, 2011
Starr DiGiacomo
Cantaloupes Doubted for Outbreak of Listeria Monocytogenes
Submitted by Neelesh Raghuwanshi on Wed, 09/28/2011 - 10:34
The cantaloupes cultivated in the region of Granada, Colorado, have been recalled for examination by the US Centers for Disease Control and Prevention, in Georgia. As per the information of the authorities, 72 people from 18 states of the US were found to be infected with the infection.
The outbreak started on August 15. Listeria monocytogenes is a bacterial disease, which results in forming lieteriosis on the body of the infected. This is the most dangerous form of food-borne disease.
According to the media, the people died due to the disease belonged to the region of Kansas, Missouri, Nebraska and Texas. The number of deaths due to the infection is believed to have outraced the mortality due to salmonella disease that occurred due to peanuts three years back. Apart from confirmation of 13 deaths due to listeria monocytogenes, another 3 people were being doubted of being in a serious condition and their chances for survival from the disease is very less.
http://topnews.net.nz/content/219179-cantaloupes-doubted-outbreak-l...
Sep 28, 2011